Research Article
Shoulder Pain Post-Laparoscopy Surgery: Ketoprofen – Tramadol Infusional Therapy
Cielo Alborada Ureña-Frausto1*, and Ricardo Plancarte-Sánchez2
1IMSS Hospital General de Zona # 6 con MF, Monterrey NL
2Servicio Clínica del Dolor, Instituto Nacional de Cancerología, México DF
Corresponding author
Dr. Cielo Alborada Ureña Frausto, IMMSS Hospital General de Zona # 6 con MF, Monterrey NL, Mexico, E-mail: cielo_urena@hotmail.com
Received Date: 18th April 2015
Accepted Date: 05th May 2015
Published Date: 08th May 2015
Citation
Ureña-Frausto CA, Plancarte-Sánchez R (2015) Shoulder Pain Post-Laparoscopy Surgery: Ketoprofen – Tramadol Infusional Therapy. Enliven: J Anesthesiol Crit Care Med 2(6): 016.
Copyright
@ 2015 Dr. Cielo Alborada Ureña Frausto. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction
Post-operative pain with difficult control, is a reality that can occur in patients undergoing laparoscopic cholecystectomy, it is good comprehensively assess the patient and give a painkiller scheme that ensures the absence of pain.
Objective
To compare the analgesic efficacy of tramadol-ketoprofen over a control group in three management schemes in infusional therapy; to control the painful entity (shoulder pain post-laparoscopy surgery).
Material and Methods
Clinical trial non-randomized; Group I (n = 15) managed with ketorolac 1mg/kg; Group II (n = 12) ketoprofen 100mg; Group III (n = 14) ketoprofen 50 mg plus tramadol 50 mg and Group IV (n = 15) ketoprofen 100 mg plus tramadol 100 mg. The variability analyzed was: Pain, pain bailouts, side effects and patient satisfaction.
Results
The highest intensity of pain was found in Group I (conventional) , unlike Group II and III where the predominant category was mild pain, the Group IV presents minimal pain events; 98% significance of p <0.01.
Conclusion
The analgesic efficiency of ketoprofen in infusional therapy is superior to the conventional administration of ketorolac; nevertheless the analgesic scheme handled with ketoprofen 100 mg plus tramadol 100 mg reaches the analgesic efficiency.
Keywords
Post-operative pain; Laparoscopic surgery; Laparoscopic cholecystectomy; Infusional therapy
Abstract
Introduction: Post-operative pain with difficult control, is a reality that can occur in patients undergoing laparoscopic cholecystectomy, it is good comprehensively assess the patient and give a painkiller scheme that ensures the absence of pain.
Objective: To compare the analgesic efficacy of tramadol-ketoprofen over a control group in three management schemes in infusional therapy; to control the painful entity (shoulder pain post-laparoscopy surgery).
Material and Methods: Clinical trial non-randomized; Group I (n = 15) managed with ketorolac 1mg/kg; Group II (n = 12) ketoprofen 100mg; Group III (n = 14) ketoprofen 50 mg plus tramadol 50 mg and Group IV (n = 15) ketoprofen 100 mg plus tramadol 100 mg. The variability analyzed was: Pain, pain bailouts, side effects and patient satisfaction.
Results: The highest intensity of pain was found in Group I (conventional) , unlike Group II and III where the predominant category was mild pain, the Group IV presents minimal pain events; 98% significance of p <0.01. Conclusion: The analgesic efficiency of ketoprofen in infusional therapy is superior to the conventional administration of ketorolac; nevertheless the analgesic scheme handled with ketoprofen 100 mg plus tramadol 100 mg reaches the analgesic efficiency.
Introduction
The International Association for the Study of Pain (acronym in English IASP) defines pain, as a sensory and emotional unpleasant experience that is associated with tissue damage, which is real or potential, or described in terms of such damage [1], by its etiology pain is classified as nociceptive and neuropathic [2]. Nociceptive pain is low threshold transmission, from mechano-receptors and primary afferent fibers that mediate tactile sensory function (somatic and visceral pain). Neuropathic pain involves neurobiological components that interact at multiple levels of the neuraxial axis.
An important risk factor to develop chronic pain after surgery is the severity of post-operative pain. Acute constant pain may appear after surgery; the lack of systematized evaluation with absence in pain documentation registries during post-operative period may conduct to an inadequate detection of it [3].
It is clearly justified the implementation of an acute pain medical team, by statistics it has been reported the death of 20.044 patients, 74% due to opioid-analgesics prescript by physicians [4]. The guidelines of acute pain evaluation and management of peri-operative pain involved institutional policies that assured a systematized and periodic evaluation with qualify personal [5].
The pain assessment should be realized with easy utilization and interpretation scales [6]. The instruction of the correct use of the pain assessment scales should be directed to patients and its families during the pre-anesthetic evaluation [7,8]. Pain intensity documentation approaches a better evaluation of therapeutic response.
The knowledge and understanding in a patient of its biological mechanisms that causes pain, help control and modulate the same pain [9]. Nociceptive system is reflected in neurophysiology and pathophysiology of the transmission and modulation of painful stimuli. Synaptic transmission afferents is modulated by GABA and glycine release from interneurons in the dorsal horn of the spinal cord [10]. Nociception is influenced by genetic factors that potentially alter the pharmacokinetic properties of the analgesic drugs, which are not specific to a mode [11].
The presence of neuropathic pain represents 71.1% in post-operative period [12]. Research on pain assessment considers the number of domains of pain, intensity, quality, location and temporal variations in the pain intensity.
In patients after laparoscopic cholecystectomy is considered the pathophysiology of the disease itself; insufflation of carbon dioxide causes shoulder referred pain; with an incidence of 76.7% [13], with re-hospitalization for shoulder pain in 41% of patients in outpatient surgeries [14]. Management guidelines recommend high quality anesthesia, use analgesia protocols individualized for each patient [15].
An infusional therapy with infusion pump (PCA) maintains regularity in the provision of products reaching a better control on the nociceptive system; preventive analgesia avoids neuronal plasticity and decreases pain hypersensitivity. A multimodal analgesia in an opioid analgesic regime adding an NSAID generates an empowering effect of all resources [16], obtaining better control in the nociceptive system, having bio equivalencies with other drugs (ketoprofen 25-100 mg equals acetaminophen 650 mg plus codeine 60 mg; tramadol 1 mg/kg IV equals acetaminophen 15 mg/kg/per day) without having so much adverse effects.
Justification
Using a multimodal analgesia individualized for each patient, providing the benefit of tramadol and ketoprofen synergism in an infusional therapy to solve the laparoscopic cholecystectomy post-operative shoulder pain, focused on improving the quality of care for the patients.
Hypothesis
The administration 60 minutes before surgery in laparoscopic cholecystectomy in the managed group with an ideal scheme of tramadol 100 mg IV plus ketoprofen 100 mg IV, continuing therapy with infusional: tramadol 0.2 mg/kg/hour plus ketoprofen 2 mg/kg/24 hours, during 24 hours postoperative achieves the analgesic efficacy in painful shoulder syndrome.
Null Hypothesis
The administration 60 minutes before laparoscopic cholecystectomy surgery in a group managed with ideal scheme: tramadol 100 mg IV plus ketoprofen 100 mg IV, continuing therapy with infusional tramadol 0.2 mg/kg/hour plus ketoprofen 2 mg/kg/24 hours for 24 hours postoperative do not reached the analgesic efficacy in painful shoulder syndrome.
Objective
General
To compare postoperative analgesic efficacy of ketoprofen and tramadol plus ketoprofen on infusional therapy vs conventional analgesic therapy in different modalities, specific to referred shoulder pain in laparoscopic cholecystectomy.
Specifics
1. To analyze the post-operative analgesic efficacy of ketorolac (conventional group) in the surgical wound (parietal and visceral) and specifically the pain in shoulder motion and motionless in laparoscopic cholecystectomy for 24 hours.
2. To analyze the postoperative analgesic efficacy of ketoprofen in the surgical wound (parietal and visceral) and specifically the pain in shoulder motion and motionless in laparoscopic cholecystectomy for 24 hours.
3. To analyze the postoperative analgesic efficacy of tramadol plus ketoprofen over two management schemes in the surgical wound (parietal and visceral) and specifically the pain in shoulder motion and motionless in laparoscopic cholecystectomy for 24 hours.
4. Identify adverse effects of the drugs under study.
Material and Methods (Non-Randomized Clinical Trial)
Selection Criteria
Patients of both sexes, aged 18 and under 70 years, body mass index (BMI) <35, elective and emergency surgery with anesthetic risk rating ASA I-II were included undergoing laparoscopic cholecystectomy. The anesthetic technique used was thoracic epidural neuraxial anesthesia T10-T11 level, using lidocaine with epinephrine 20 mg/0.0025mg/ml (15 ml), the second dose with bupivacaine 5 mg/ml (7.5ml). Excluded patients were the ones with a previous analgesic management scheme that skew the study; psychiatric, septic, hematologic or hepatic disease patients; patient’s background use of anticoagulants or antidepressants; allergic reaction to any of the drugs used in the study as well as contraindication to neuraxial anesthesia.
The sample size calculation was based on proportions of 60 patients, who were divided in four groups of 15 patients in each group; however due to a mechanical failure in laparoscopic equipment, only 56 surgeries were performed.
Measurement of the Main Variables
The measured variables in the study were: Age, sex, surgical wound pain (parietal, visceral) and specifically shoulder pain (motion and motionless), tramadol rescue dosage, side effects (nausea, vomiting, sweating, dizziness or drowsiness) and patient satisfaction.
Procedure
The groups were assigned as non-randomized, in all patients thoracic epidural neuro-axial anesthesia was used, Group I received analgesia scheduled (conventional), Groups II, III and IV received intravenous infusional therapy with infusion pump Terumo Corporation. (Terfusion infusion pump TE 171, Tokyo Japan, Europe 3001 Leven NV Belgium) preventive analgesia was administrated in the four groups, 60 minutes before surgery.
• Group I (n=15) ketorolac 1 mg/kg in 100 ml of saline 0.9% (maximum dose to the ideal weight of the patient) at the end of surgery ketorolac 30 mg every 8 hours for 24 hours. (Conventional).
• Group II (n=12) ketoprofen 100 mg in 100 ml of saline solution and implementing individualized dose per kilo of weight infused with ketoprofen 2 mg/kg/24hours in 1000 ml of 0.9% saline for 24 hours.
• Group III (n=14) tramadol 50 mg plus ketoprofen 50 mg plus in 100 ml of saline solution; implementing an individualized infusion dose per kilo of weight with tramadol 0.1mg/kg/hour plus ketoprofen 1 mg/kg/24 hours in 1000 ml of 0.9% saline solution for 24 hours.
• Group IV (n=15) tramadol 100 mg plus ketoprofen 100 mg in 100 ml of saline solution; implementing an individualized infusion dose per kilo of weight with tramadol 0.2 mg/kg/hour plus ketoprofen 2 mg/kg/24 hours in 1000 ml of 0.9% saline solution for 24 hours.
Patients with no satisfactory VAS results (greater than 3) needed to be administrated a tramadol 50 mg IV rescue dose as required.
Assessment of Pain
1. During the pre-anesthetic evaluation instructions are given to the patients regarding the scales of pain which they are going to be evaluate: Visual Analog Scale (Table 1) and pain category (Table 2), also the characteristics of pain to be evaluate were explain: Parietal pain (define as superficial pain in the surgical wound), visceral pain (deep pain which correspond to abdominal cavity). Both kinds of pain were evaluated at 0, 1, 2, 4, 6, 8 and 24 hours.
2. Shoulder pain specifically to scapular level motion and motionless at 0, 1, 2, 4, 6, 8 and 24 hours, using the same scales explained before.
3. Evaluation of associated variables: Nausea, vomiting, dizziness, drowsiness and sweating.
4. Patient satisfaction.
5. Rescues doses with tramadol.
Table 1. Visual Analog Pain Scale (VAS)
|
Grade |
Pain |
|
0 |
No Pain |
|
1 |
Mild |
|
2 |
Moderate |
|
3 |
Severe |
Pain Categories
Table 2. Pain Categories
Statistical Analysis
Record sheets were designed for the study development, the general characteristics of the population were described using measures of central tendency and dispersion using frequencies and ranges in qualitative and mean and standard deviation for quantitative.
To prove our hypothesis we used a non-parametric test Kruskal-Wallis based in the sample size due to the existence of more than two unpaired groups, considering a statistically significant when p value is <0.05. Even though the sample size is limiting, the results were significant.
Results
A total of 56 patients were included in the study: 87.5% female patients (49 patients) and 12.5% male patients (7 patients). The age groups of patients have a percentage distribution as follows: 0-16 years 0%, 17-50 years 82% and over 50 years 18%. Population was divided into four treatment groups’ regardless sex or age, as follows: Group I: 15 patients (27%) Group III: 12 patients (21%), Group III: 14 patients (25%) and Group IV: 15 patients (27%). The physical state of patients according to the classification of the American Society of Anesthesiology (ASA) was: ASA I: 42 patients and ASA II: 14 patients (75% and 25%). We performed pain assessment with Categorical Pain Scale and Visual Analog Scale (VAS) in parietal and visceral surgical pain and shoulder pain specifically without movement and movement for 24 hours post-operative with the following results:
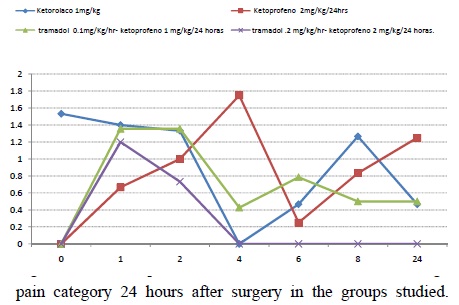
1. Motionless Shoulder pain: Group I: 15% (Severe 53%, Moderate 40% , Mild 7%), Group II: 20% (Severe 10%, Moderate 25% and Mild 65%), Group III: 20% (Severe 10%, Moderate 30% Mild 60%), Group IV: 5% (Severe 20%, Moderate 60% and Mild 20%). At movement subtle changes were found.
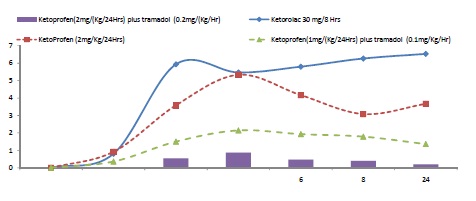
2. Motion Shoulder pain: Group I: 15% (Severe 33%, Moderate 60% and Mild 7%), Group II: 22% (Severe 9%, Moderate 27% and Mild 64%), Group III: 20% (Severe 10%, Moderate 30% and Mild 60%), Group IV: 5% (Severe 20%, Moderate 60% and Mild 20%). (Table 3, Figure1 and Figure 2).
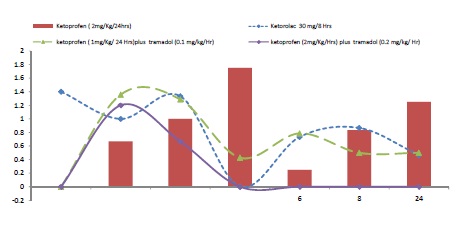
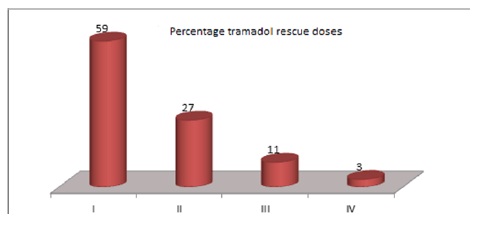
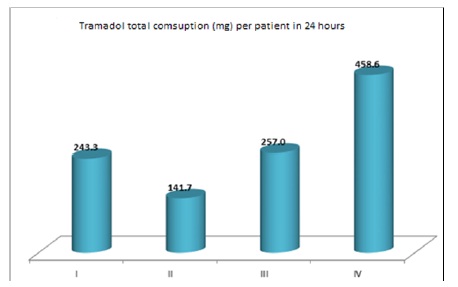
3. The total rescue doses with tramadol 50 mg in the study groups was 124, of which were received: Group I 59%, Group II 27%, Group III 10% and Group IV 3% (Figure 3).
4. Motionless visceral pain: Group I: 39% ( Severe 56%, Moderate 28%, Mild 15%), Group II 40% (Severe 13%, Moderate 50% and Mild 37%), Group III: 33% (Severe 3%, Moderate 0% and Mild 97%) , Group IV: 3% (Severe 0%, Moderate 0%, Mild 100%).
5. Motion visceral pain: Group I: 62% (Severe 65%, Moderate 29% and Mild 6%), Group II: 58% (Severe 29%, Moderate 45% and Mild 26%) , Group III: 51% (Severe 4%, Moderate 4% and Mild 92%), Group IV: 19% (Severe 0%, Moderate 0% and Mild 100%).
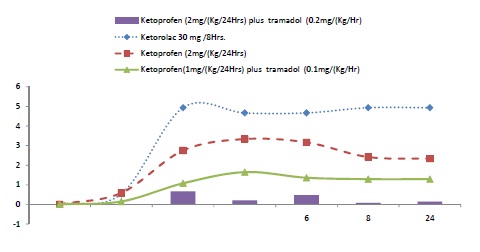
6. The frequency of greatest pain presents in movement in patients of Group I with an average VAS 8-9 at 2, 4, 6, 8 and 24 hours; at a time in patients of Group II predominates Moderate Pain Category with VAS 4-5, in Group III was predominated Mild pain and Group IV reaches no pain. (Figure 4).
7. Motionless parietal pain: Group I: 39% (Severe 49%, Moderate 18% and Mild 33%), Group II: 20% (Severe 5%, Moderate 10%, Mild 85%), Group III: 27% (Severe 0%, Moderate 0% and Mild 100%), Group IV: 4% (Severe 0%, Moderate 0%, Mild 100%).
8. Motion parietal pain: Group I: 48% (Severe 73%, Moderate 21% and Mild 6%), Group II: 43% (Severe 30%, Moderate 38% and Mild 42%), Group III: 36% (Severe 3%, Moderate 3% and Mild 94%), Group IV: 12% (Severe 0%, Moderate 0%, Mild 100%). With movement, 12% of patients presented pain (Severe 0%, Moderate 0% and Mild 100%). The greater frequency of pain occurs with movement in parietal pain (Severe Pain Category Group I), 73% of patients achieving at 2 hours post-operative assessment an average VAS of 9. (Figure 5).
9. Tramadol consumption per group: Group I: 3650 mg (243.3 mg consumption per patient within 24 hours), Group II: 1700 mg (141.6 mgs consumption per patient within 24 hours), Group III: 3598 mg (257 mg consumption per patient within 24 hours.), Group IV: 6879 mg (458.6 mg consumption per patient within 24 hours) (Figure 6).
10. Side effects: Nausea and vomiting Group I with 40%, Group III 29%, Group IV with 20%, and Group II with 14% of patients. Diaphoresis and sweating were presented in Group I and III in 7% of patients in each group. Drowsiness was presented in Group I and III in 20 and 21%, and in group IV: 13%, the group II only in 8% of patients.
11. The degree of patient satisfaction: Group IV very good, Group III and II good in 100% of patients unlike of the patients of Group I in which 60% of patients expressed dissatisfaction at the end of 24 hours. The fatigue-related upper limb shoulder pain occurred in two patients of Group I (13%).
12. Study differences in pain or gender Shoulder pain gender: Both men and women differences in pain with or without movement are not significant. In men, 80% experienced moderate to severe pain in group 3.In Women: Group 1, 29% experienced moderate to severe pain. Group 2, 31% experienced mild to moderate pain, Group 3, 31% experienced mild pain and Group 4 only 10% experienced mild to moderate pain. Statistically shoulder pain; women are more sensitive to pain than man, under the circumstances of the study (Table 4).
13. Visceral pain gender: In men, 31% of mild to moderate pain occurred in Group 2, and 69% mild pain occurred in Group 3.In women: Group 1, 42% experienced moderate to severe pain. Group 2, 32% experienced mild to moderate pain. Group 3, 23% experienced mild to moderate pain. Group 4 only 3% experienced mild pain without movement and at movement 12% of patients experimented mild pain. Visceral pain according to the results is stronger in women than men (Table 5).
14. Gender parietal pain: In men, mild to moderate pain occurred in 50% of patents in Group 2, mild pain in 38% of patients in Group 3 and mild pain in 13% of patients in Group 4.In women, Group 1, 51% of patients experienced moderate to severe pain. Group 2, 23% experienced moderate to severe pain at movement. Group 3, 26% experienced mild pain. Group 4 only 4% experienced mild pain without moving and at movement 10% of patients’ experienced mild pain. Parietal pain according to the results is stronger in women than in men. (Table 6).
Figure 1. Shoulder pain without movement (SPWOM), average pain category 24 hours after surgery in the groups studied.
Figure 2. Shoulder pain with movement (SPWM), average pain category 24 hours after surgery in the studied groups.
Figure 3. Tramadol rescue doses 24 hours after surgery in the studied groups.
Figure 4. Visceral pain with movement (Analog Visual Scale), 24 hours after surgery in the studied groups.
Figure 5. Visceral pain without movement (VPWOM) (Analog Visual Scale), 24 hours after surgery in the studied groups.
Figure 6. Total tramadol usage by patient in mg, 24 hours after surgery.
|
WMPS |
MPS |
|||||||
|
Pain Scale |
Group |
Group |
||||||
|
I |
II |
III |
IV |
I |
II |
III |
IV |
|
|
Mild |
7 |
65 |
60 |
20 |
7 |
64 |
60 |
20 |
|
Moderate |
40 |
25 |
30 |
60 |
60 |
27 |
30 |
60 |
|
Severe |
53 |
10 |
10 |
20 |
33 |
9 |
10 |
20 |
|
No Pain |
85 |
80 |
80 |
95 |
85 |
78 |
80 |
95 |
Table 3. Average pain categories
WMPS = Without movement pain shoulder
MPS = Movement pain shoulder
They defined for this study patients with laparoscopic cholecystectomy surgery and were included in the sample in its natural sequence of arrival. 87.5% of all patients who underwent surgery were women and 12.5% men.
| PAIN INTENSITY | SHOULDER PAIN WITHOUT MOVEMENT | SHOULDER PAIN WITH MOVEMENT | ||||||||||||||||||
| Nª | AGE | WM PS0 |
WM PS1 |
WM PS2 |
WM PS4 |
WM PS6 |
WM PS8 |
WMP S24 |
AVER AGE |
MP S0 |
MP S1 |
MP S2 |
MP S4 |
MP S6 |
MP S8 |
MP S24 |
AVE RAGE |
|||
| Gpo | Men/Totals | 7 | 48 | 5 | 5 | 6 | 7 | 6 | 5 | 5 | 6 | 7 | 6 | |||||||
| 1 | ketorolac 30 mg /8 Hrs | 1 | 34 | 0 | 0 | |||||||||||||||
| 2 | ketoprofen 2 mg/kg /24 Hrs | 2 | 47 | 4 | 4 | 4 | 4 | |||||||||||||
| 3 | ketrprofen (1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 3 | 47 | 5 | 5 | 7 | 7 | 6 | 5 | 5 | 7 | 7 | 6 | |||||||
| 4 | ketrprofen (2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 1 | 69 | 0 | 0 | |||||||||||||||
| Women/Totals | 49 | 37 | 8 | 4 | 4 | 4 | 3 | 4 | 3 | 4 | 7 | 4 | 4 | 4 | 3 | 4 | 6 | 5 | ||
| 1 | ketorolac 30 mg /8 Hrs | 14 | 34 | 8 | 7 | 4 | 7 | 5 | 7 | 6 | 7 | 5 | 7 | 6 | 4 | 7 | 6 | |||
| 2 | ketoprofen 2 mg/kg p/24 Hrs | 10 | 33 | 3 | 4 | 5 | 3 | 3 | 2 | 3 | 3 | 4 | 5 | 3 | 3 | 5 | 4 | |||
| 3 | ketrprofen (1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 11 | 36 | 4 | 3 | 2 | 2 | 3 | 4 | 3 | 2 | 2 | 3 | |||||||
| 4 | ketroprofen (2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 14 | 42 | 3 | 6 | 4 | 6 | 5 | 6 | |||||||||||
| Grand Total | 56 | 38 | 8 | 4 | 4 | 4 | 4 | 5 | 4 | 7 | 4 | 4 | 4 | 4 | 4 | 6 | ||||
| NUMBER OF EVENTS | SHOULDER PAIN WITHOUT MOVEMENT | SHOULDER PAIN WITH MOVEMENT | ||||||||||||||||||
| Nª | AGE | WM PS0 |
WM PS1 |
WM PS2 |
WM PS4 |
WM PS6 |
WM PS8 |
WM PS24 |
% | MP S0 |
MP S1 |
MP S2 |
MP S4 |
MP S6 |
MP S8 |
MP S24 |
% | |||
| Gpo | Men/Totals | 7 | 48 | 1 | 1 | 2 | 1 | 5 | 1 | 1 | 2 | 1 | 5 | |||||||
| 1 | ketorolac 30 mg /8 Hrs | 1 | 34 | 0% | 0% | |||||||||||||||
| 2 | ketoprofen 2 mg/kg /24 Hrs | 2 | 47 | 1 | 20% | 1 | 20% | |||||||||||||
| 3 | ketrprofen (1 mg/kg/24 Hr), + tramadol(0.1 mg/Kg/Hr) | 3 | 47 | 1 | 1 | 1 | 1 | 80% | 1 | 1 | 1 | 1 | 80% | |||||||
| 4 | ketrprofen (2 mg/kg/24 Hr) + tramadol(0.2 mg/Kg/Hr) | 1 | 69 | 0% | 0% | |||||||||||||||
| Women/Totals | 98 | 37 | 3 | 13 | 14 | 7 | 5 | 6 | 4 | 52 | 3 | 13 | 14 | 7 | 6 | 5 | 4 | 52 | ||
| 1 | ketorolac 30 mg /8 Hrs | 28 | 34 | 3 | 3 | 3 | 1 | 4 | 1 | 29% | 3 | 3 | 3 | 2 | 3 | 1 | 29% | |||
| 2 | ketoprofen 2 mg/kg /24 Hrs | 20 | 33 | 3 | 3 | 4 | 1 | 2 | 3 | 31% | 3 | 3 | 4 | 1 | 2 | 3 | 31% | |||
| 3 | ketrprofen (1 mg/kg/24 Hr), + tramadol(0.1 mg/Kg/Hr) | 22 | 36 | 4 | 6 | 3 | 3 | 31% | 4 | 6 | 3 | 3 | 31% | |||||||
| 4 | ketrprofen (2 mg/kg/24 Hr) + tramadol(0.2 mg/Kg/Hr) | 28 | 42 | 3 | 2 | 10% | 3 | 2 | 10% | |||||||||||
| Grand Total | 105 | 38 | 3 | 14 | 14 | 7 | 6 | 8 | 5 | 3 | 14 | 14 | 7 | 7 | 7 | 5 | ||||
Table 4. Shoulder pain gender:
Both men and women differences in pain with or without movement are not significant.
In men, 80% experienced moderate to severe pain in group 3.
In Women: Group 1, 29% experienced moderate to severe pain.
Group 2, 31% experienced mild to moderate pain.
Group 3, 31% experienced mild pain.
Group 4 only 10% experienced mild to moderate pain.
Statistically shoulder pain; women are more sensitive to pain than man, under the circumstances of the study.
| INTENSIDAD DE DOLOR | DOLOR VISERAL SIN MOVIMIENTO | DOLOR VISERAL CON MOVIMIENTO | |||||||||||||||||
| Nª | DV SM0 |
DV SM1 |
DV SM2 |
DV SM4 |
DV SM6 |
DV SM8 |
DV SM24 |
Prom | DV CM0 |
DV CM1 |
DV CM2 |
DV CM4 |
DV CM6 |
DV CM8 |
DV CM24 |
Prom | |||
| Gpo | Hombres/Totales | 7 | 3 | 3 | 2 | 2 | 2 | 2 | 2 | 3 | 4 | 3 | 3 | 2 | |||||
| 1 | ketorolaco 30 mg /8 Hrs | 1 | 0 | 0 | |||||||||||||||
| 2 | ketoprofeno 2 mg/kg p/24 Hrs | 2 | 5 | 1 | 1 | 1 | 2 | 5 | 3 | 4 | 1 | 3 | |||||||
| 3 | ketrprofeno(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 3 | 3 | 3 | 3 | 2 | 3 | 3 | 2 | 3 | 3 | 3 | 3 | 3 | 3 | ||||
| 4 | ketrprofeno(2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 1 | 0 | ||||||||||||||||
| Mujeres/Totales | 49 | 5 | 6 | 5 | 4 | 5 | 5 | 5 | 4 | 6 | 5 | 5 | 5 | 5 | |||||
| 1 | ketorolaco 30 mg /8 Hrs | 14 | 6 | 8 | 6 | 5 | 7 | 8 | 7 | 6 | 7 | 7 | 7 | 7 | 8 | 7 | |||
| 2 | ketoprofeno 2 mg/kg p/24 Hrs | 10 | 3 | 5 | 5 | 5 | 4 | 3 | 4 | 4 | 7 | 7 | 6 | 4 | 4 | 5 | |||
| 3 | ketrprofeno(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 11 | 4 | 2 | 2 | 2 | 2 | 2 | 3 | 5 | 3 | 2 | 2 | 2 | 3 | ||||
| 4 | ketrprofeno(2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 14 | 1 | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | ||||||||
| Grand Total | 56 | 5 | 6 | 5 | 4 | 4 | 4 | 4 | 6 | 5 | 5 | 4 | 5 | ||||||
| NUMERO DE EVENTOS | DOLOR VISERAL SIN MOVIMIENTO | DOLOR VISERAL CON MOVIMIENTO | |||||||||||||||||
| Nª | DV SM0 |
DV SM1 |
DV SM2 |
DV SM4 |
DV SM6 |
DV SM8 |
DV SM24 |
% | DV CM0 |
DV CM1 |
DV CM2 |
DV CM4 |
DV CM6 |
DV CM8 |
DV CM24 |
% | |||
| Gpo | Hombres/Totales | 7 | 1 | 3 | 3 | 3 | 3 | 13 | 1 | 1 | 4 | 4 | 4 | 5 | |||||
| 1 | ketorolaco 30 mg /8 Hrs | 1 | 0% | 0% | |||||||||||||||
| 2 | ketoprofeno 2 mg/kg p/24 Hrs | 2 | 1 | 1 | 1 | 1 | 31% | 2 | 2 | 1 | 2 | 37% | |||||||
| 3 | ketrprofeno(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 3 | 1 | 2 | 2 | 2 | 2 | 69% | 1 | 1 | 2 | 2 | 3 | 3 | 63% | ||||
| 4 | ketrprofeno(2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 1 | 0% | 0% | |||||||||||||||
| Mujeres/Totales | 98 | 4 | 18 | 22 | 18 | 17 | 19 | 98 | 6 | 26 | 35 | 34 | 33 | 31 | |||||
| 1 | ketorolaco 30 mg /8 Hrs | 28 | 2 | 9 | 8 | 7 | 7 | 8 | 42% | 2 | 12 | 12 | 13 | 13 | 13 | 39% | |||
| 2 | ketoprofeno 2 mg/kg p/24 Hrs | 20 | 2 | 4 | 7 | 6 | 5 | 7 | 32% | 3 | 6 | 8 | 8 | 8 | 10 | 26% | |||
| 3 | ketrprofeno(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 22 | 4 | 5 | 5 | 5 | 4 | 23% | 1 | 4 | 9 | 9 | 8 | 6 | 22% | ||||
| 4 | ketrprofeno(2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 28 | 1 | 2 | 3% | 4 | 6 | 4 | 4 | 2 | 12% | ||||||||
| Grand Total | 105 | 4 | 19 | 25 | 21 | 20 | 22 | 7 | 27 | 39 | 38 | 37 | 36 | ||||||
Table 5. Visceral pain gender:
In men, 31% of mild to moderate pain occurred in group 2, and 69% mild pain occurred in group 3.
In women: Group 1, 42% experienced moderate to severe pain.
Group 2, 32% experienced mild to moderate pain.
Group 3, 23% experienced mild to moderate pain.
| PAIN INSTENSITY | PARIETAL PAIN WITHOUT MOVEMENT | PARIETAL WITH MOVEMENT | |||||||||||||||||
| Nª | WM PP0 |
WM PP1 |
WM PP2 |
WM PP4 |
WM PP6 |
WM PP8 |
WM PP24 |
AVER AGE |
MP P0 |
MP P1 |
MP P2 |
MP P4 |
MP P6 |
MM P8 |
MM P24 |
AVER AGE |
|||
| Gpo | Men/Totals | 7 | 2 | 3 | 3 | 2 | 4 | 2 | 2 | 3 | 3 | 2 | 3 | 2 | |||||
| 1 | ketorolac 30 mg /8 Hrs | 1 | |||||||||||||||||
| 2 | ketoprofen 2 mg/kg /24 Hrs | 2 | 2 | 3 | 4 | 1 | 3 | 2 | 2 | 3 | 1 | 3 | 1 | 2 | |||||
| 3 | ketrprofen(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 3 | 2 | 2 | 3 | 2 | 2 | 2 | 3 | 2 | |||||||||
| 4 | ketrprofen (2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 1 | 3 | 3 | 3 | 3 | |||||||||||||
| Women/Totals | 49 | 8 | 5 | 5 | 4 | 4 | 5 | 5 | 7 | 6 | 5 | 5 | 5 | 5 | 5 | ||||
| 1 | ketorolac 30 mg /8 Hrs | 14 | 8 | 8 | 6 | 6 | 7 | 8 | 7 | 8 | 8 | 7 | 7 | 7 | 7 | 8 | |||
| 2 | ketoprofeno2 mg/kg /24 Hrs | 10 | 4 | 3 | 4 | 2 | 3 | 3 | 5 | 8 | 6 | 6 | 4 | 5 | 6 | ||||
| 3 | ketrprofen(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 11 | 2 | 3 | 2 | 2 | 2 | 2 | 3 | 3 | 3 | 3 | 3 | 3 | |||||
| 4 | ketrprofen (2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 14 | 3 | 3 | 3 | 2 | 2 | 2 | 1 | 1 | 2 | ||||||||
| Total | 56 | 5 | 5 | 5 | 4 | 4 | 5 | 5 | 4 | 6 | 5 | 5 | 5 | 5 | 5 | ||||
| NUMBER OF EVENTS | PARIETAL PAIN WITHOT MOVEMENT | PARIETAL PAIN WITH MOVEMENT | |||||||||||||||||
| Nª | WM PP0 |
WM PP1 |
WM PP2 |
WM PP4 |
WM PP6 |
WM PP8 |
WM PP24 |
% | MP P0 |
MP P1 |
MP P2 |
MP P4 |
MP P6 |
MP P8 |
MP P24 |
% | |||
| Gpo | Men/Totals | 7 | 1 | 2 | 1 | 1 | 1 | 2 | 8 | 2 | 2 | 1 | 2 | 2 | 3 | 12 | |||
| 1 | ketorolac 30 mg /8 Hrs | 1 | 0% | 0% | |||||||||||||||
| 2 | ketoprofen 2 mg/kg/24 Hrs | 2 | 1 | 1 | 1 | 1 | 50% | 1 | 1 | 1 | 1 | 2 | 2 | 67% | |||||
| 3 | ketorprofen(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 3 | 1 | 1 | 1 | 38% | 1 | 1 | 1 | 25% | |||||||||
| 4 | ketorprofen(2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 1 | 1 | 13% | 1 | 8% | |||||||||||||
| Women/Totals | 98 | 1 | 15 | 14 | 18 | 17 | 15 | 2 | 22 | 25 | 26 | 24 | 23 | ||||||
| 1 | ketorolac 30 mg /8 Hrs | 28 | 1 | 8 | 8 | 8 | 8 | 8 | 51% | 1 | 9 | 10 | 10 | 10 | 10 | 41% | |||
| 2 | ketoprofen 2 mg/kg p/24 Hrs | 20 | 2 | 2 | 3 | 4 | 2 | 16% | 1 | 4 | 6 | 6 | 6 | 5 | 23% | ||||
| 3 | ketrprofen(1 mg/kg/24 Hr), + Tramadol(0.1 mg/Kg/Hr) | 22 | 3 | 4 | 6 | 5 | 5 | 29% | 6 | 7 | 6 | 7 | 6 | 26% | |||||
| 4 | ketrprofen (2 mg/kg/24 Hr) + Tramadol(0.2 mg/Kg/Hr) | 28 | 2 | 1 | 4% | 3 | 2 | 4 | 1 | 2 | 10% | ||||||||
| Totals | 105 | 2 | 17 | 15 | 19 | 18 | 17 | 88 | 4 | 24 | 26 | 28 | 26 | 26 | 134 | ||||
Table 6. Gender parietal pain:
In men, mild to moderate pain occurred in 50% of patents in group 2, mild pain in 38% of patients in group 3 and mild pain in 13% of patients in group 4.
In women, Group 1, 51% of patients experienced moderate to severe pain.
Group 2, 23% experienced moderate to severe pain at movement.
Group 3, 26% experienced mild pain.
Group 4 only 4% experienced mild pain without moving and at movement 10% of patients’ experienced mild pain.
Parietal pain according to the results is stronger in women than in men.
|
Group |
Somnolence and |
Sweating and |
Vomiting |
|||
|
dizziness |
diaphoresis |
|||||
|
No |
% |
No |
% |
No |
% |
|
|
I |
3 |
20 |
1 |
7 |
6 |
40 |
|
II |
1 |
8 |
0 |
0 |
2 |
14 |
|
III |
3 |
21 |
1 |
7 |
4 |
29 |
|
IV |
2 |
13 |
0 |
0 |
3 |
20 |
|
total |
9 |
16 |
2 |
4 |
15 |
27 |
Table 7. Adverse Effects in group studies
Discussion
Perioperative pain in laparoscopic cholecystectomy leads to a multimodal analgesic approach integrating preventive analgesia to a synergism ketoprofen plus tramadol infusional therapy [17].
Ambulatory Surgery Centers has a 10% higher return compared to hospitals with outpatient care [18]. The decrease in hospital stay has great economic benefits [19] but nevertheless; the possibility of integrating laparoscopic cholecystectomy in patients of Ambulatory Surgery Centers generates controversia [20]. The incidence of pain mentioned in several studies; as reports Waitayawinyu P; with the presence of post-operative pain moderate to severe intensity in 76.7%, to studies of Jacob AK et al. [13], where reports a hospital re-admission for shoulder pain in 41% of patients in surgery ambulatory [14]. Hospital Centers priority and commitment to achieve quality of life (no pain) and satisfaction in all patients difficult this procedures to be programmed in Ambulatory Surgery Centers.
In groups of patients similar to our study, Castillo-Garza G et al. [21], administered during the trans-operative preventive analgesia with bupivacaine 0.5%, obtained post-operative analgesia for 6 hours [21]. The group study of Bucciero M et al. [22] administered intraperitoneal nebulization’s with ropivacaine 1% reaches absent of pain. Studies Murphy GS et al. [23] founded favorable results administrating dexamethasone 8 mg before and after surgery, achieving post-operative analgesia. Zhang H et al. [24] with multiple doses of parecoxib achieve a decrease incidence of pain from 61.9% to 24.4%. In a similar population to ours, studies Gögenur I et al. [25] used melatonin 5 mg showing no difference with the placebo group.
Another important factor to determinate perioperative analgesia is Obstructive Sleep Apnea, which has a prevalence of 3% to 7% in men and 2% to 5% in women [26,27]. The use of opioids reaches a higher incidence of respiratory depression during the perioperative period: 3.6 per 10,000 adult patients (0.038%), Jarzyna D, et al. [28,29].
Opioid´s use during general anesthesia leads to a respiratory depression which demands closer follow up. IV tramadol infusion (week opioid) is associated with a higher risk of respiratory depression, nausea, vomiting, pruritus and deeper sedation; less frequent apnea and midriasis and possible mechanism of respiratory depression may occur in presence on liver and renal damage [30,31]. In conclusion analgesic benefits are higher than adverse effects. Regarding ketoprofen, it is consider to be a drug with a high therapeutic index, and not necessary to monitories it blood levels [32,33]. Also, we found that as the other NSAID the permanent consumption may cause cardiovascular and gastrointestinal risks; ketoprofen inhibits COX and blocks prostaglandins at peripheral and central level [34]. Activation at peripheral level and in medulla of 5-HT2bR serotonin receptor may be implied the favorable effects or anti-nociceptive effects [35]. In our study the dosage of tramadol and ketoprofen are in safety levels and attended to the security guidelines, both drugs reaches therapeutic effects with the minimum of adverse effects.
In this study we seek choosing an analgesic scheme, which conserves the respiratory function [17]. The choice of anesthetic technique is critical to good control of pain because it determines a successful recovery [36,37], as evidenced by the group Tripathi DC, where reported during the trans-operative hemodynamic response that impacts during the post-operative period [38]. These studies demonstrated the need for a multimodal analgesia.
There is a significant difference in pain score in the three groups with different management schemes compared with the conventional group. Analgesia with infusional therapy for limited periods with home care can be provided with the support of an available specialist nurse. The studies as well as various studies show evidence of a suitable analgesic requirement hospital or outpatient basis, at least in the first 24 hours post-surgery. If we consider the current biopsychosocial conceptualization examines the impact of pain on daily living activity [39], we can achieve great benefit to our patients if this analgesic was handled as an ideal scheme and be applied in outpatient hospital centers to ensure painless post-operative period.
In this study 87.5% of all patients who underwent surgery were women and 12.5% men, they defined for this study patients with laparoscopic cholecystectomy surgery and were included in the sample in its natural sequence of arrival; despite the difference in number of patients in Group, the results coincide with the results of Tighe PJ cols [40]. Statistically shoulder pain; Gender parietal pain, Gender parietal pain women are more sensitive to pain than man, under the circumstances of the study.
Conclusions
In laparoscopic cholecystectomy shoulder pain during the postoperative period in 24 hours with conventional management are difficult to control, it causes distress in patients where there’s really not enough treatment and analgesia must be implemented. Ketoprofen analgesic efficacy in infusional therapy is superior to conventional management with ketorolac. Severe pain in surgical wound at movement was present using the analgesic scheme tramadol 0.1mg/kg/hour plus ketoprofen 1 mg/kg/24 hours. The infusional therapy with 100 mg ketoprofen plus tramadol 100 mg in 100 ml of saline, 60 minutes prior to surgery and starting intravenous infusion tramadol 0.2 mg/kg/hour plus ketoprofen 2mg/ kg/24 hours in 1000 ml of saline 0.9% reach the analgesic efficacy safely and can be a good alternative to treat this painful entity.
References
- IAS bibliography P Task Force on Taxonomy. Part III (1994) The pain terminology. En: Classification of Chronic Pain Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. Second Edition. Seattle Washington. ISAP Press 209-214.
- (1986) Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 3: S1-226.
- Te Boveldt ND, Vernooij-Dassen MJ, Jansen A, Vissers KC, Engels Y (2015) Pain is not systematically Registered in Dutch Medical Oncology Outpatients. Pain Pract 15: 364-370.
- Upp J, Kent M, Tighe PJ (2013) The Evolution and Practice of Acute Pain Medicine. Pain Med 14: 124-144.
- Rabah Heresi E Dolor Postoperatorio Guías de Dolor agudo FEDELAT (Federación Latinoamericana de Sociedades de Dolor) 2:10-30
- Schofield PA (2014) The assessment and management of peri-operative pain in older Adult Anaesthesia 69: 54-60.
- Ayón-Villanueva H (2011) Perioperative management of pain in cancer patients. Rev Mex Anest 34: S68-S71.
- Guevara LU, Covarrubias GA, Hernández A (2004) Parámetros development of practice for the management of acute pain. Rev Mex Anest 27: 200-204.
- Catley MJ, O’Connell NE, Moseley GL (2013) How Good Is the Neurophysiology of Pain Questionnaire? A Rasch Analysis of Psychometric Properties. J Pain 14: 818-827.
- Mukhida K, Mendez M, Mcleod I, Kobayashi N, Haughn C, et al. (2012) Spinal GABAergic Transplants Attenuate Mechanical Allodynia in a Rat Model of Neuropathic Pain. Stem Cells 25: 2874-2885.
- Smith MT, Muralidharan A (2012) Review Pharmacogenetics of pain and analgesia. Clin Genet 82: 321-330.
- Casale R, Mattia C (2014) Building a diagnostic algorithm on localized neuropathic pain (LNP) and targeted topical treatment: focus on 5% lidocaine-medicated plaster. Ther Clin Risk Manag 10: 259-268.
- Waitayawinyu P, Siriwannasandha B, Namwong A (2012) Incidence and Risk Factors of Moderate to Severe Pain in 24 hours after Laparoscopic Cholecystectomy. SMJ 64: 119-122.
- Peng PW, Farcas CL, Haley A, Wong W, Bender J, et al. (2010) Use of low-dose pregabalin in patients undergoing laparoscopic cholecy stectomy. Br J Anaesth 105: 155-161.
- Griffiths R, Beech F, Brown A, Dhesi J, Foo I, et al. (2014) Guidelines Peri-operative care of the elderly 2014, Association of Anaesthetists of Great Britain and Ireland. Anaesthesia 69: 81-98.
- The British Pain Society, the Royal College of Nursing and the Royal College of Paediatrics and Child Health (2012) Good Practice in Postoperative and Procedural Pain Management 2nd Edition, 2012 Pediatric Anesthesia 1: 1-79.
- Ureña-Frausto C, Plancarte-Sánchez R, Reyes-Torres JI, Ramírez-Aranda JM (2013) Terapia infusional: una alternativa en dolor de hombro post-laparoscopía. Cir Cir 81: 187-191.
- Plotzke MR, Courtemanche C (2011) Does procedure profitability impact whether an outpatient surgery is performed at an ambulatory surgery center or hospital? Health Econ 20: 817-830.
- Vuilleumier H, Coquelin G, Wasserfallen JB, Demartines N (2011) Cost - Effective Utilization of a Private Facility to Perform Outpatient Surgery in Public Hospital Waiting List Patients. Dig Surg 28: 299-303.
- Zilvetti M, Puttick M, Parameswaran R, Mcwhinnie D (2010) Day Surgery and National Tariff: Is There Room for Economic Sense? The Journal of One Day Surgery 19: 64-67.
- Castillo-Garza G, Díaz-Elizondo JA, Cuello-García CA, Villegas-Cabello O (2012) Irrigation with Bupivacaine at the Surgical Bed for Postoperative Pain Relief after Laparoscopic Cholecystectomy. JSLS 16: 105-111.
- Bucciero M, Ingelmo PM, Fumagalli R, Noll E, Garbagnati A, et al. (2011) Intraperitoneal Ropivacaine Nebulization for Pain Management after Laparoscopic Cholecystectomy: A Comparison with Intraperitoneal Instillation. Anesth Analg 113: 1266-1271.
- Murphy GS, Szokol JW, Greenberg SB, Avram MJ, Vender JS, et al. (2011) Preoperative dexamethasone enhances quality of recovery after laparoscopic cholecystectomy: effect on in-hospital and postdischarge recovery outcomes. Anesthesiology 114: 882-890.
- Zhang H, Shu H, Yang L, Cao M, Zhang J, et al. (2012) Multiple- But Not Single-, Dose of Parecoxib Reduces Shoulder Pain after Gynecologic Laparoscopy. Int J Med Sci 9: 757-765.
- Gögenur I, Kücükakin B, Bisgaard T, Kristiansen V, Hjortsø NC, et al. (2009) The Effect of Melatonin on Sleep Quality after Laparoscopic Cholecystectomy: A Randomized, Placebo-Controlled Trial. Anesth-Anal 108: 1152-1156.
- Park JG, Ramar K, Olson EJ (2011) Updates on Definition, Consequences, and Management of Obstructive Sleep Apnea. Mayo Clin Proc 86: 549-555.
- Punjabi NM (2008) The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc 5: 136-143.
- Jarzyna D, Jungquist CR, Pasero Ch, Willens JS, Nisbet A, et al. (2011) American Society for Pain Management Nursing Guidelines on Monitoring for Opioid - Induced Sedation and Respiratory Depression. Pain Manag Nurs 12: 118-145.
- Ramachandran SK, Haider N, Saran KA, Mathis M, Kim J, et al. (2011) Life-threatening critical respiratory events: A retrospective study of postoperative Patients found unresponsive during analgesic therapy. J Clin Anesth 23: 207-213.
- Macintyre PE, Scott DA, Schug SA, Visser EJ, Walker SM (2010) Acute Pain Management: Scientific Evidence Australian and New Zealand. College of Anaesthetists and Faculty of Pain Medicine.
- Makris A, Matala ME, Tsirigotis A, Karmaniolou I (2012) Apnea and mydriasis after postoperative tramadol administration: an unusual complication and possible underlying mechanisms. Anaesthesia 67: 76-77.
- Delage N, Maaliki H, Beloeil H, Benhamou D, Mazoit JX (2005) Median Effective Dose (ED50) of Nefopam and Ketoprofenin Postoperative PatientsA Study of Interaction Using Sequential Analysis and Isobolographic Analysis. Anesthesiology 102: 1211-1216.
- Kantor TG (1986) Ketoprofen A review of its pharmacology and clinics properties Pharmacotherapy 6: 93-103.
- De Beaurepaire R, Suaudeau C, Chait A, Cimetière C (1990) Anatomical mapping of brain sites involved in the antinociceptive effects of ketoprofen. Brain Res 536: 201-216.
- Urtikova N, Berson N, Steenwinckel JV, Doly S, Truchetto J, et al. (2012) Antinociceptive effect of peripheral serotonin 5-HT2B receptor activation on neuropathic pain. Pain 153: 1320-1331.
- Unic-Stojanovic D, Babic S, Jovic M (2012) Benefits, risks and complications of perioperative use of epidural anesthesia. Med Arch 66: 340-343.
- Mitra S, Khandelwal P, Roberts K, Kumar S, Vadivelu N (2012) Pain Relief in Laparoscopic Cholecystectomy—A Review of the Current Options. Pain Pract 12: 485-496.
- Tripathi DC, Shah KS, Dubey SR, Doshi SM, Raval PV (2011) Hemodynamic stress response during laparoscopic cholecystectomy: Effect of two different doses of intravenous clonidine premedication.J Anaesthesiol Clin Pharmacol 27: 475-480.
- Mendoza ME, Gertz KJ, Jensen MP (2014) Contributions of four pain domains to the prediction of patient functioning and pain interference. Psychol Neurosci 7: 3-8.
- Tighe PJ, Riley JL, Fillingim RB (2014) Sex Differences in the Incidence of Severe Pain Events Following Surgery: A Review of 333,000 Pain Scores. Pain Med 15: 1390-1404.