Case Report
Severe Unilateral Atelectasis after Induction of General Anesthesia: Due to Aspiration of Oropharyngeal Secretion?
Myoung Jin Ko, MD*, Sujung Lee, MD, Sang Eun Lee, MD, Ki Wha Lee, MD, Sang Yoon Jeon, MD, and Jae Hong Park, MD*
Department of Anesthesiology and Pain Medicine, Haeundae Paik Hospital, Inje University, Busan, South Korea
Corresponding author
Jae Hong Park, MD, Assistant professor, Department of Anesthesiology and Pain Medicine, Haeundae Paik Hospital, Inje University, Busan, South Korea, Tel: +82-51-797-0422; Fax: +82-51-797-0499; E-mail: H00150@paik.ac.kr
Received Date: 29th September 2014
Accepted Date: 29th October 2014
Published Date: 31st October 2014
Citation
Ko MJ, Lee S, Lee SE, Lee KW, Jeon SY, et al. (2014) Severe Unilateral Atelectasis after Induction of General Anesthesia: Due to Aspiration of Oropharyngeal Secretion? Enliven: J Anesthesiol Crit Care Med 1(5): 013.
Copyright
@ 2014 Dr. Jae Hong Park. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, that permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
A 27-year-old man underwent general anesthesia for arthroscopic Bankart repair surgery. Glycopyrrolate was administered for premedication and anesthesia was induced with propofol and rocuronium. After tracheal intubation, the patient’s position was changed to right lateral position for operation. Gradual elevation of airway pressure and decrease of oxygen saturation occurred, and was suspected to be due to endobrochial intubation. Nonetheless, the endotracheal tube was drawn to 22 cm at the upper incisor and breathing sound was not auscultated overthe right lung field. Bronchoscopy was performed for diagnosis, right main bronchus was filled withclear mucus secretion. After suction of the secretion, ventilation was improved. After finishing the operation, a chest X-ray showed aspiration pneumonia overthe right lung. The patient was treated with antibiotics and discharged uneventfully 5 days postoperatively.
Keywords
Atelectasis; Aspiration pneumonia; General anesthesia
Abstract
A 27-year-old man underwent general anesthesia for arthroscopic Bankart repair surgery. Glycopyrrolate was administered for premedication and anesthesia was induced with propofol and rocuronium. After tracheal intubation, the patient’s position was changed to right lateral position for operation. Gradual elevation of airway pressure and decrease of oxygen saturation occurred, and was suspected to be due to endobrochial intubation. Nonetheless, the endotracheal tube was drawn to 22 cm at the upper incisor and breathing sound was not auscultated over the right lung field. Bronchoscopy was performed for diagnosis, right main bronchus was filled withclear mucus secretion. After suction of the secretion, ventilation was improved. After finishing the operation, a chest X-ray showed aspiration pneumonia overthe right lung. The patient was treated with antibiotics and discharged uneventfully 5 days postoperatively.
Introduction
Intraoperative atelectasis during general anesthesia is common. Pulmonary atelectasis may be caused by a variety of factors [1]. However, severe unilateral atelectasis that causes increasing airway pressure and severe hypoxemia is rare. In this case, the patient underwent general anesthesia, developed severe hypoxemia after position change. Diagnostic bronchoscopy showed clear mucus secretion blocking right main bronchus and removal of secretion improved ventilation. After operation, a chest X-ray showed aspiration pneumonia over right lung field. Atelectasis may have occurred due to aspiration of oropharyngeal secretion.
Case Report
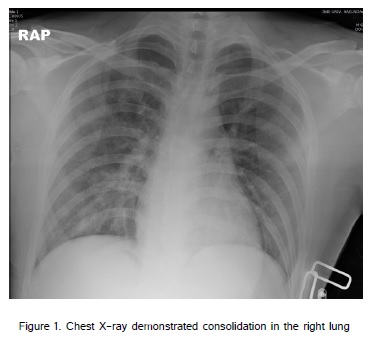
A 27-year-old man (height 185 cm, weight 90 kg) suffering from Bankart lesion at left shoulder was scheduled for arthroscopic Banrkart repair surgery. He had a smoking history (1 pack/day for 7years) and other medical history was unremarkable. Preoperative laboratory data, chest X-ray and electrocardiogram were normal. The patient had not orally consumed food for over 8 hours. Gycopyrrolate 0.2 mg was administered intravenously for secretion reduction preoperatively. The peripheral artery oxygen saturation (SpO2), electrocardiogram, non-invasive blood pressure and end tidal carbon dioxide (EtCO2) were monitored in the operation room. Anesthesia was induced with propofol 120 mg and after confirming loss of consciousness, rocuronium 50 mg was administered for muscle relaxation. One minute after rocuronium administration, the patient hiccupped and then additive rocuronium 20 mg was administered. Mask ventilation and tracheal intubation were achieved smoothly and there were little secretion in oral cavity. Respiratory sounds were readily audible in bilateral lung field and the endotracheal tube was fixed at 23cm upper incisor. Anesthesia was maintained with desflurane and remifentanil infusion at 0.1mcg/kg/min. We changed the patient to right lateral position for the operation. A few minutes after position change, gradual elevation of peak airway pressure from 17 mmHg to 35 mmHg occurred and SpO2 dropped to 90%. The endotracheal tube was deepened to 25cm. We suspected endobronchial intubation and pulled out the tube to 22 cm at upper incisor, but there was no respiratory sound in right lateral lung field. In spite of ventilation with fraction of inspired oxygen (FiO2) 1.0, SpO2 dropped to 83 %. The patient’s position was returned to supine and emergent bronchoscopy was performed for diagnosis. Correct endotracheal tube positioning was confirmed. No gastric contents, foreign bodies and abnormalities of airway were observed in the trachea. When the bronchoscope (KARL STORZ 11301 AA1 intubation fiberscope, 2.8 mm outer diameter, Germany) entered the right main bronchus, there was large amount of clear mucus secretion blocking the bronchus completely. The secretion was aspirated using a suction port with bronchoscopy guidance. The secretion was clear and sticky. After aspiration, wheezing was auscultated in the right lung field and we treated with salbutamol inhalation, after which the rale sound was auscultated in right lung field. The peak airway pressure decreased to 20 mmHg and SPO2was elevated above 90 %. Arterial blood gas analysis (ABGA) showed pH 7.29, PCO2 58 mmHg and PO2 77mmHg.The patient became stable and his position was changed to right lateral. The operation commenced. The ventilation improved during operation, SpO2 was 100% with 0.5 FiO2. After the operation was complete, muscle relaxation was reversed with sugamadex 180 mg, sevoflurane and remifentanil administration were discontinued. The patient’s cooperation was good and extubation was done uneventfully. ABGA after the extubation showed pH 7.33, PCO2 50 mmHg and PO2 106 mmHg.The patient was transferred to the postanesthetic care unit and there was no symptom such as cyanosis or dyspnea and SPO2 was 95% in room air. Postoperative chest X-ray demonstrated consolidation over right lung, and impression was aspiration pneumonia (Figure 1). The patient was transferred to the general ward and treated with antibiotics. Postoperative day 4, we visited the patient. There was no fever or dyspnea and respiratory sound and ABGA were normal. Postoperative day 5, the patient was discharged uneventfully without any other complaints or respiratory symptoms.
Discussion
The notable finding in this case is that severe unilateral atelectasis occurred due to mucus secretion, which blocked the main bronchus in a healthy, young patient who had no underlying disease. Complete blockade of right bronchus by the secretion lead to significant hypoxia and impaired ventilation. Despite FiO2 1.0 application, desaturation was ongoing. In case of V/Q mismatch, hypoxia can be corrected by oxygen supply. So we suspected that the hypoxia was caused by true shunt, rather than a V/Q mismatch. Intraoperative pulmonary shunt is caused by pneumonia, intracardiac shunt and atelectasis. In our case, we suspected that the atelectasis caused hypoxia. Bronchial secretion is a frequent cause of atelectasis and segmental or lobar collapse often results from bronchial obstruction by secretion. Preoperative pulmonary infection, smoking and immobility are the risk factors for perioperative pulmonary atelectasis [2,3]. However, atelectasis during general anesthesia occurs usually as microatelectasis in the alveoli in the dependent lung and severe atelectasis, as in this case, is rare [1]. Kainkaryam et al. [4] reported severe unilateral atelectasis during induction of anesthesia in an 11-year-old female and diagnosed as bronchomalacia postoperatively. Bronchomalacia often affects children, but our patient was an adult free of anatomical abnormalities.
Sudden airway obstruction is usually caused by anesthetic breathing system malposition, endobronchial intubation, asthma and pneumothorax. After exclusion of these causes, we performed bronchoscopy for diagnosis. Large amount of secretion blocked right main bronchus and after suctioning this secretion, ventilation was improved. Therefore we confirmed a diagnosis of right total atelectasis due to airway obstruction by the secretion. Similarly, Igarashi et al. [5] reported pulmonary atelectasis after induction of anesthesia due to airway obstruction by secretion. In their case, the patient was diagnosed as sinobronchial syndrome postoperatively. Sinobronchial syndrome can induce airway hypersecretion. However, our patient had no history of sinusitis, no risk factors of airway hypersecretion except for the history of smoking. We used anticholinergics as premedication for antisialogogue effect; different from the case of Igarashi et al. [5]; unfortunately, the secretion’s components were not analyzed, so we could not confirm that the origin was from bronchus or oropharynx.
The chest X-ray taken postoperatively demonstrated consolidation in the right lung and the impression was aspiration pneumonia. It will be difficult to identify the exact time when aspiration occurred. Given the characteristics of cuff sealing and positive pressure ventilation, there is little chance for aspiration of oropharyngeal secretion after complete muscle relaxation with additional muscle relaxant administration. In our opinion, the aspiration was probably done by hiccups and mask ventilation before endotracheal intubation was performed. We believe that aspiration occurred only at the level of trachea and upper airway because of gentle mask ventilation. At the supine position, secretion probably lied evenly at the upper airway level. We estimate the airway diameter was large enough that it was not blocked by the secretion. Due to postural changes, secretion probably moved to the dependent lung, involving airway obstruction and desaturation. Perioperative aspiration pneumonia is a potentially fatal complication of anesthesia. Abdominal surgery, emergency surgery, obesity, pregnancy and diabetes mellitus increase the risk of aspiration and when large amount of acidic gastric contents are aspirated, significant lung damage can occur [6]. In our case, the patient had none of these risk factors and had consumed nothing by mouth for over 8 hours. The patient hiccupped during induction of anesthesia and we suspected aspiration of gastric contents at that time. However, his oral cavity was clean when we intubated the endotracheal tube and there was no gastric content or foreign body but secretion in the bronchoscopic view. Perioperative microaspiration of contaminated oropharyngeal secretion can cause aspiration pneumonia [7]. However, it usually occurs among patients who receive long-term ventilator care at intensive care units. In short operations like our case, it rarely occurs. As we surmised, incognizant oropharyngeal secretion was aspirated to lungs before endotracheal intubation. Anesthesiologists always should be aware of unexpected aspiration and cautions for sufficient preoxygenation, sedation and muscle relaxation are required. Rapid sequence induction and cricoid pressure are useful for the patient with high risk ofaspiration [8]. Use of modified cuff shape endotracheal tube is helpful to prevent intraoperative microaspiration [9].
In summary, we report a case of severe unilateral atelectasis after induction of general anesthesia. When sudden hypoxia or impaired ventilation occurs during anesthesia, anesthesiologists should check anesthetic breathing system, endotracheal tube malposition and breathing sounds preferentially. Prompt diagnostic bronchoscopy should be helpful when diagnosis is ambiguous.
References
8) Birmacombe JR, Berry AM (1997) Cricoid pressure. Can J Anaesth 44: 414.