Research Article
Glycaemic Control, and Associated Practices among Diabetic Patients in Private Practice: A Focus on Rubaga Hospital, A Private Tertiary Hospital in Uganda
Magoola Andrew Patrick1, Kibuule Dan2*, Kagoya Harriet Rachel3, Rugera Simon Peter1, and Mitonga Kabwebwe Honoré4
1Department of Medical Laboratory Sciences, Faculty of Medicine, Mbarara University of Science and Technology, Mbarara Uganda
2Head of Department Pharmacy practice & lecturer pharmacotherapy, University of Namibia, Faculty of Health Sciences, School of Pharmacy, Box 13301, 340 Mandume Ndemufayo Avenue Pioneers park, Windhoek, Namibia
3Public Health Specialist and Monitoring and evaluation specialist, Management Sciences for Health, Namibia
4Senior Lecturer Epidemiology and Biostatistics, University of Namibia, Faculty of Health Sciences, School of Medicine, Namibia
Corresponding author
Kibuule Dan, B Pharm, MSc, Clinical Pharmacology, Head of Department Pharmacy practice & lecturer pharmacotherapy, University of Namibia, Faculty of Health Sciences, School of Pharmacy, Box 13301, 340 MandumeNdemufayo Avenue Pioneers park, Windhoek, Namibia, Tel: +264 61-206 5048; +264 (0) 81-628 0835; E-mail: dkibuule@unam.na, kibuulefamily@yahoo.co.uk
Received Date: 15th April 2015
Accepted Date: 14th May 2015
Published Date: 18th May 2015
Citation
Patrick MA, Kibuule D, Kagoya HR, Rugera SP, Kagoya HR (2015) Glycaemic Control, and Associated Practices among Diabetic Patients in Private Practice: A Focus on Rubaga Hospital, A Private Tertiary Hospital in Uganda. Enliven: Pharmacovigil Drug Saf 2(2): 004.
Copyright
@ 2015 Kibuule Dan. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, that permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The control of blood glucose is critical in prevention of complication of diabetes and to improve the quality of life of these patients. However in a setting of patients attending care from a private setting, the access to inexpensive care may be a critical control of diabetes, a life-long chronic illness that requires optimal adherence to nutritional and medication. Such practices may ultimately heighten the financial burden associate with management of diabetes of complications such as hypertension and diabetic foot. In spite of this, the Glycaemic control practices in private health care settings in Uganda have not been well described and thus may negatively impact on the health outcomes.
The study aimed to describe the practices among diabetic patients attending the Rubaga hospital, determine the level of Glycaemic control and identify the factors associated with diabetics’ patients monitoring indicators (Hb1Ac levels, blood glucose levels).
This is a Cross-sectional analytical study.
Patients were randomly selected during the period of April and May 2012. The laboratory determination of the blood glucose levels (RBG) and Glycosylated hemoglobin (HB1AC) was done using the COBAS 6000 clinical chemistry analyser. Analysis was done using the student T-test and Chi-square test with a level of significance of 0.05.
There was a significant statistical relationship between fasting plasma glucose and HbA1c (p-value = 0.000). Factors influencing high HBA1C levels in diabetic patients at Rubaga hospital were high cost of diabetes mellitus treatment (p-value = 0.019), duration the study participant had had the disease (P = 0.003) and having another chronic illness alongside diabetes mellitus (p-value = 0.045).
The Republic of Uganda should make treatment of diabetes mellitus universally accessible and free. It should also put sensitization measures in place geared towards minimizing occurrence of some chronic disease conditions like hypertension which lead to co-treatment that lowers drug compliance.
Keywords
Glycaemic control; Practices; Diabetes; Rubaga; Uganda
Abstract
The control of blood glucose is critical in prevention of complication of diabetes and to improve the quality of life of these patients. However in a setting
of patients attending care from a private setting, the access to inexpensive care may be a critical control of diabetes, a life-long chronic illness that requires optimal adherence to nutritional and medication. Such practices may ultimately heighten the financial burden associate with management of diabetes of complications such as hypertension and diabetic foot. In spite of this, the Glycaemic control practices in private health care settings in Uganda have not been well described and thus may negatively impact on the health outcomes.
The study aimed to describe the practices among diabetic patients attending the Rubaga hospital, determine the level of Glycaemic control and identify
the factors associated with diabetics’ patients monitoring indicators (Hb1Ac levels, blood glucose levels).
This is a Cross-sectional analytical study.
Patients were randomly selected during the period of April and May 2012. The laboratory determination of the blood glucose levels (RBG) and
Glycosylated hemoglobin (HB1AC) was done using the COBAS 6000 clinical chemistry analyser. Analysis was done using the student T-test and Chisquare test with a level of significance of 0.05.
There was a significant statistical relationship between fasting plasma glucose and HbA1c (p-value = 0.000).
Factors influencing high HBA1C levels in diabetic patients at Rubaga hospital were high cost of diabetes mellitus treatment (p-value = 0.019), duration
the study participant had had the disease (P = 0.003) and having another chronic illness alongside diabetes mellitus (p-value = 0.045).
The Republic of Uganda should make treatment of diabetes mellitus universally accessible and free. It should also put sensitization measures in place
geared towards minimizing occurrence of some chronic disease conditions like hypertension which lead to co-treatment that lowers drug compliance.
Introduction
Diabetes has of recent become a major health burden in Uganda, with over million people affected and 8.1% of subpopulations in Kampala and Mukono districts [1]. More than 28.9% patients with diabetes mellitus in Uganda have poor access to quality care, medication and are non-compliant to treatment recommendations [2]. In Uganda, patients with diabetes in search for cure of the disease, consult both conventional and traditional medical treatments. Health seeking practices of consulting multiple health providers may impact negatively of Glycaemic control as some modalities have not been validated.
Though the glycated hemoglobin (HbA1c) is the recommended test for monitoring glycaemic control for the up to 6 to 8 weeks, most health facilities in Uganda routinely use the random blood glucose (RBG) assessments [3].Thus the status the Glycaemic control for most patients attending private hospitals such as Rugaba may be unknown and thus lead to unknown treatment outcomes.
Practices to improve glycaemic control among patients receiving care at private health facilities has not been fully explored, thus factors such as; gender and age of the patient [4-7]; adherence to prescribed medication and clinic appointments [8,9]; comorbidities related pill burden [10] quality of diabetes care by provider, [11] whereas [12], patient satisfaction and multi professional care [13] and the costs of [14], influence the HbA1c levels.
Methods and Materials
Design and Setting
Mixed, descriptive cross-sectional and experimental designs were employed to determine the fasting blood glucose (FBG) and HbA1c and glycaemic control practices among diabetic out patients attending Rubaga hospital. Rubaga hospital with a 300 bed capacity, is a private not for profit faith based hospital, under the Catholic arch diocese of Kampala serves a catchment area of Kampala, Wakiso, Mpigi, Mukono districts.
Study Population and Sampling
The study population included all diabetic patients attending the out-patient clinic of Rubaga hospital with a known history of diabetes treatment of more than 6 weeks. Ninety six (96) patients [15] were recruited into the study using simple random sampling. Uniformly sized cards numbered with numbers 1 to192 were enclosed in a box for selection. Only patients picking numbers 1-96 were recruited into the study upon obtaining informed consent.
Data Collection and Management
Data was collected by the principal researcher, who is also a laboratory technologist. The study questionnaires were pre-tested and standardized. Upon consenting to participate in the study, patients were interviewed to complete the questionnaires on their glycaemic control practices and knowledge. History of the last meal was taken to ascertain the whether the blood sugar was fasting or random.
Following the interview, a blood specimen was obtained from the patient for FBG and HbA1c analysis. All blood specimens were collected in fluoride containers to minimize glycolysis which influences the FBG results. Controls were used to validate the results for each specimen using a COBAS 6000 clinical chemistry analyser- HBA1C <6.0% meant good glycaemic control while that of >6.0% meant poor glycaemic control
All questionnaires were serialized and validated for completeness. Quantitative data was entered in Epidata v3.1 software for management and exported to SPSS v21 software for analysis. Categorical data was analyzed using Pearson chi-square test and continuous data using the T test.
Ethical Considerations
The study was approved by Mbarara University Research and Ethics committee and institutional research committee of Rubaga hospital. Only patients who consented were included in the study and their identifiers were not included, rather questionnaires were coded.
The participation of the study subject was voluntary after receiving explanation on the intended study aims, risks, benefits of the study and confidentiality was guaranteed. The participants signed an informed consent form agreeing to participate voluntarily in the study. This consent form and procedure was approved by the Ethical Committee.
Results
Ninety six (96) patients were participated in the study among them 39 (40.6%) participants were 46 to 60 years of age, 34 (35.4%) were over 60 years and 23 (24.0%) were 18 to 45years of age. Seventy five (78.1%) of the study participants were female and 21 (21.9%) were male.49 (51.0%) of the study participants were primary school drop outs, 25 (26.0%) were secondary school drop outs, 14 (14.6%) had attained tertiary education and 8 (8.3%) were completely illiterate. 55 (57%) of the study participants were peasants, 30 (31%) were business persons, 8 (9%) were civil servants and 3 (3%) were unemployed.
Twenty three (23) of the study participants who had glucose levels of less than 110mg/dl, 16 (69.6%) had normal HbA1c values of less than 6% and 7 (30.4%) had values greater than 6.0%. Of the 23 participants with glucose values of 110-140mg/dl, 11 (47.8%) had HbA1c values of less than 6.0% and 12 (52.2%) had values greater than 6.0%. The results further showed that of the 27 study participants with fasting blood glucose of 140-200mg/dl, 18 (66.7%) had HbA1c values of greater than 6.0% and 9 (33.3%) had one less than 6.0%. It is further revealed in that of the 23 study participants with fasting plasma glucose levels above 200mg/dl, 21 (91.3%) had HbA1c levels above 6.0 and only 2 (8.7%) had HbA1c levels below 6.0%.
The results further indicated that 35.3% of the study participants who had lived with diabetes mellitus for less than a year, 48.5% of those that had lived with the disease for 1 to 5years, 35.0% of those with it for 6 to 10 years and 34.6% of the ones who had had the disease for more than 10years had HbA1c levels of less than 6%. HBA1C levels for those with recent diagnosis of diabetes mellitus to those of patients with a long history of having the disease were comparable with no significant variation (p = 0.81).
The results revealed that among the 23 study participants who were 18 to 45years of age, 9 (39.1%) had HbA1c of less than 6.0% and 14 (60.9%) had it greater than 6.0%. Of the 39 participants aged 46 to 60year old, 15 (38.5%) had HbA1c of less than 6.0% and 24 (61.5%) had one of greater than 6.0%. The table further shows that of the 34 study participants aged over 60years, 14 (41.2%) had HbA1c of less than 6.0% and 20 (58.2%) had it greater than 6.0%. HBA1C levels were comparable in all age groups (p = 0.833).
The results related to the study participant’s level of education attained and their glycated haemoglobin levels presented that of the 49 study participants who stopped at primary education, 26 (53%) had HbA1c above 6.0% and 12 (47%) had it less than 6.0%. Of the 25 who had stopped at secondary level of education, 13 (52%) had HbA1c levels above 6.0% and 12 (48%) had values less than 6.0%. It is further revealed that for the 14 study participant who had attained tertiary education, 13 (92.9%) had HbA1c levels above 6.0% and 1 (7.1%) had values less than 6.0%. A similar pattern was revealed in the 8 study participants who were illiterate where, 6 (75%) had HbA1c levels above 6.0% and 2 (25%) had the levels below 6.0%. No systematic trend was observed about HBA1C levels based on level of education and hence no statistically significant relationship could be inferred from this (p = 0.426).
About the duration spent between last DM treatment doses related with HbA1c levels of the study participants, we found that duration spent without taking treatment of diabetes mellitus never revealed a definite significant trend with HBA1C levels of the study participants (p = 0.325). Of the 49 study participants who had taken their DM treatment that same day, 31 (63.3%) had HbA1c levels above 6.0% and 18 (36.7%) had levels below 6.0%, a similar trend with similar percentages for the 30 study participants who had missed treatment for about a day or two. The trend was reversed for the 11 participants of more than a week off treatment for DM who instead had 8 (72.7%) of them having HbA1c levels below 6.0% and 3 (27.3%) had it greater than 6.0%. For the 6 participants who had spent 3 to 7days off DM treatment, 5 (83.3%) had HbA1c levels above 6.0% and 1 (16.7%) had the levels less than 6.0%.
The results about missing of drug taking and Hb1Ac levels of study participants exposed that of the 82 study participants that never missed taking medication even once, 48 (58.5%) had HbA1c levels above 6.0% and 34 (41.5%) had the levels below 6.0%. It further reveals that of the 14 who at times missed taking treatment for DM, 10 (71.4%) had HbA1c values greater than 6.0% and 4 (28.6%) had values less than 6.0%. Hence, HBA1C levels of participants who at times failed to take medication for diabetes mellitus were comparable to those of participants who always regularly took their medication (p = 0.494).
Regarding the reason for the study participants failing to take DM medication at times, the results indicated that 82 (86%) of the study participants were always adherent to medication, 5 (5%) failed to take the medication because they were tired of taking it, 3 (3%) failed be because of poor timing which made them forget taking it, 3 (3%) was because of drug stock outs, 2 (2%) did so to allow their herbal remedies to work 1 (1%) did it because they felt well enough not to take the medicine.
On the type of medication and Hb1Ac levels of study participants the study showed that of the 82 study participants on oral hypoglycaemics alone for DM treatment, 46 (56.1%) had HbA1c levels above 6.0% and 36 (43.9%) had the levels below 6.0%. All the 4 (100%) on both oral plus parenteral hypoglycaemics had HbA1c levels above 6.0% whereas of the 10 participants on only parenteral hypoglycaemics, 8 (80%) had HbA1c levels above 6.0% and 2 (20.0%) had the levels below 6.0%. There was no statistically significant relationship between type of treatment for diabetes mellitus and glycaemic control based on HBA1C levels (p= 0.144).
Regarding taking of co-medication for another chronic illness and Hb1Ac levels of the study participants the results revealed that 60 study of participants who were taking co-medication for another chronic illness, 40 (66.7%) had HbA1c levels above 6.0% and 20 (33.3%) had the levels below 6.0%. The table further shows that of the 36 participants who were not taking co-medication for another chronic illness, there were as many having HbA1c above 6.0% as there were those with the value below 6.0%, which was 50.0%. HbA1c levels were higher in people taking medication for other chronic illness alongside that diabetes mellitus than in those on treatment for only diabetes mellitus (p = 0.045).
Concerning the distribution of other chronic diseases among the study participants, showed that 55 (57.3%) of the study participants were on treatment for hypertension, 36 (37.5%) were not on treatment for any chronic disease condition, 2 (2.1%) were on ARV treatment, 2 (2.1%) were on peptic ulcer disease treatment and 1 (1.0%) was on tuberculosis treatment.
The DM medication treatment fatigue and HbA1c levels of the study participants showed that drug fatigue among the study participants was not associated with poor glycaemic control (p = 0.877). Of the 84 study participants who felt that they were not tired or fatigued with the treatment of DM, 51 (60.7%) had HbA1c levels above 6.0% and 33 (39.3%) had the levels below 6.0%. Of the 12 participants who at times felt tired of taking the medication for DM, 7 (58.3%) had HbA1c levels above 6.0% and 5 (41.7%) had the levels below 6.0%.
About the adverse effect of DM treatment among the participants and their Hb1Ac levels shows that of the 73 study participants without adverse effects of DM treatment, 45 (61.6%) had HbA1c levels above 6.0% and 28 (38.4%) had the levels below 6.0%. Further on, it is revealed that of the 23 participants who were experiencing adverse effects of DM treatment, 13 (56.5%) had HbA1c levels above 6.0% and 10 (43.5%) had the levels below 6.0%. Based on the findings in this table, having adverse effects of drugs for DM treatment was not associated with poor glycaemic control (P = 0.86). The use of herbal treatment alongside medical prescriptions for DM treatment and HbA1c values of the study participants revealed that using herbs for DM treatment alongside medical prescriptions was not associated with high HBA1C levels (p = 0.348). Of the 75 study participants who were only using medically prescribed treatment, 46 (61.3%) had HbA1c levels above 6.0% and 29 (38.7%) had the levels below 6.0%. The table further reveals that of the 21 participants using herbs for DM treatment alongside medical prescriptions, 12 (57.1%) had HbA1c levels above 6.0% and 9 (42.9%) had the levels below 6.0%.
BMI and HbA1c values of the study participants showed that of the 68 overweight or obese study participants by BMI classification, 40 (58.8%) had HbA1c levels above 6.0% and 28 (41.2%) had the levels below 6.0%. It was further revealed that of the 28 study participants that were normal or underweight by BMI classification, 18 (64.3%) HbA1c levels above 6.0% and 10 (35.7%) had the levels below 6.0%. Obesity was not a predisposing factor of poor glycaemic control defined by HBA1C levels above 6% (p = 0.598).
On the duration of having DM and FBS levels of study participants showed that the longer one had lived with DM, the higher were their chances of having elevated or high fasting blood glucose (P = 0.003). Of the 33 study participants who had had DM for 1 to 5 years, 21 (63.6%) had fasting blood glucose concentration of over 110mg/dl and 12 (36.4%) had it under 110mg/dl. Of the 26 participants who had had the disease for more than 10years, 25 (96.2%) had fasting blood glucose concentrations of over 110mg/dl and 1 (3.8%) had it under 110mg/dl. The table further shows that of the 20 participants who had had DM for 6 to 10years, 15 (75%) had fasting blood glucose concentration of over 110mg/dl and 5 (25%) had it under 110mg/dl with a similar trend registered in those who had had the disease for less than a year where, 12 (70.6%) of the participants had fasting blood glucose concentration of over 110mg/dl and 5 (29.4%) had it under 110mg/dl.
Finally the results showed that the 36 (53.7%), 18 (72%) and 4 (100%) study participants who rated the cost of diabetes mellitus treatment as expensive, affordable and cheap respectively had HbA1c levels above 6.0%. Glycaemic control deteriorated with perceived increase in costliness of treatment by the study participant (P = 0.019). This makes perceived increased cost of treatment by the participants a predisposing factor to poor glycaemic control (HbA1c levels >6.0%).
Distribution of the Respondents by Demographic Characteristics (n =96)
(Table 1)
| Xteristic | Sex | Total (n= 96) | *P value | |
| Male (n= 21) | Female (n =75) | |||
| Age of Patient (years) | ||||
| 18 – 45 years | 6 | 17 | 23 | 0.438 |
| 46-60 years | 9 | 30 | 39 | |
| > 60 years | 6 | 28 | 34 | |
| Marital status | ||||
| Married or Cohabiting | 21 | 34 | 55 | 0 |
| Widowed or Divorced | 0 | 24 | 24 | |
| Not married | 0 | 17 | 17 | |
| Highest Education level | ||||
| None | 0 | 8 | 8 | 0 |
| Primary | 4 | 45 | 49 | |
| Secondary | 8 | 17 | 25 | |
| Tertiary | 9 | 5 | 14 | |
| Occupation status | ||||
| Peasant | 4 | 51 | 55 | 0 |
| Civil servant | 4 | 4 | 8 | |
| Business person | 11 | 19 | 30 | |
| Unemployed | 2 | 1 | 3 | |
| Body Mass Index (BMI) | ||||
| Underweight (< 18) | 2 | 0 | 2 | 0.006 |
| Normal (18-25) | 26 | 18 | 26 | |
| Overweight (35-30) | 25 | 19 | 25 | |
| Obese (>30) | 43 | 38 | 43 | |
Table 1: Distribution of study respondents by socio-demographic characteristics (n =96)
*P value determined by Pearson chi-square test
Distribution of Respondent by Blood Glucose Control (n =96)
(Table 2)
| Xteristic | Sex | Total (n= 96) | *P value | |
| Male (n= 21) | Female (n =75) | |||
| Blood Glucose (mg/dL) | ||||
| 110 mg/dl | 7 | 16 | 23 | 0.665 |
| 110-140 mg/dl | 2 | 21 | 23 | |
| 140-200mg/dl | 8 | 19 | 27 | |
| > 200mg/dl | 4 | 19 | 23 | |
| HbA1c % | ||||
| < 6% | 7 | 31 | 38 | 0.703 |
| 6-10% | 10 | 29 | 39 | |
| > 10% | 4 | 15 | 19 | |
| Years with diabetes | ||||
| < 1 year | 5 | 12 | 17 | 0.247 |
| 1 to 5 years | 8 | 25 | 33 | |
| 6 to 10 years | 4 | 16 | 20 | |
| > 10 years | 4 | 22 | 26 | |
Table 2: Distribution of study respondents by blood glucose and Glycosylated hemoglobin level
*P value determined by Pearson chi-square test
Factors Influencing HB1Ac Levels in Diabetic Patients at Rubaga Hospital (n=96)
(Table 3)
| Xteristic | Glycosylatedhemoglobin (HbA 1c) | Total (n= 96) | *P value | ||
| < 6% | 6% - 10% | > 10% | |||
| Blood Glucose (mg/dL) | |||||
| 110 mg/dl | 16 | 7 | 0 | 23 | 0 |
| 110-140 mg/dl | 11 | 6 | 6 | 23 | |
| 140-200mg/dl | 9 | 16 | 2 | 27 | |
| > 200mg/dl | 2 | 10 | 11 | 23 | |
| Years with diabetes | |||||
| < 1 year | 6 | 5 | 6 | 17 | 0.81 |
| 1 to 5 years | 16 | 13 | 4 | 33 | |
| 6 to 10 years | 7 | 11 | 2 | 20 | |
| > 10 years | 9 | 10 | 7 | 26 | |
| Age of Patient (years) | |||||
| 18 – 45 years | 9 | 11 | 3 | 23 | 0.833 |
| 46-60 years | 15 | 15 | 9 | 39 | |
| > 60 years | 14 | 13 | 7 | 34 | |
| Highest Education level | |||||
| None | 2 | 3 | 3 | 8 | 0.426 |
| Primary | 23 | 18 | 8 | 49 | |
| Secondary | 12 | 8 | 5 | 25 | |
| Tertiary | 1 | 10 | 3 | 14 | |
| Date of last medication dose | |||||
| Today | 18 | 22 | 9 | 9 | 0.325 |
| 1-2 days back | 11 | 13 | 6 | 6 | |
| 3-7 days back | 1 | 2 | 3 | 3 | |
| > 1 week back | 8 | 2 | 1 | 1 | |
| Ever fails to take medication | |||||
| Yes | 4 | 7 | 3 | 14 | 0.494 |
| No | 34 | 32 | 16 | 82 | |
| Type of Medication | |||||
| Oral hypoglycemic | 36 | 31 | 15 | 82 | 0.144 |
| Oral plus parenteral | 0 | 2 | 2 | 4 | |
| Parenteralonly | 2 | 6 | 2 | 10 | |
| Patient taking co-medication | |||||
| Yes | 20 | 28 | 12 | 60 | 0.045 |
| No | 18 | 11 | 7 | 36 | |
| Medication Fatigue | |||||
| Yes | 5 | 4 | 3 | 12 | 0.877 |
| No | 33 | 35 | 16 | 84 | |
| Experiencing Adverse effects | |||||
| Yes | 10 | 7 | 6 | 23 | 0.86 |
| No | 28 | 32 | 13 | 73 | |
| Use of Local medicines | |||||
| Yes | 9 | 10 | 2 | 21 | 0.348 |
| No | 29 | 29 | 17 | 75 | |
| Body Mass Index (BMI) | |||||
| Underweight (< 18) | 2 | 0 | 0 | 2 | 0.598 |
| Normal (18-25) | 8 | 10 | 8 | 26 | |
| Overweight (35-30) | 12 | 8 | 5 | 25 | |
| Obese (>30) | 16 | 21 | 6 | 43 | |
Table 3: Factors associated with Hb1Ac levels among diabetic patients at Rubaga
*P value determined by Pearson chi-square test
Factors Associated with Blood Glucose Levels (n =96)
(Table 4)
| Xteristic | Blood Glucose level (mg/dl) | Total (n= 96) | *P value | |||
| <110 | 110-140 | 140-120 | >200 | |||
| Years with diabetes | ||||||
| < 1 year | 5 | 4 | 6 | 2 | 17 | 0.003 |
| 1 to 5 years | 12 | 9 | 8 | 4 | 33 | |
| 6 to 10 years | 5 | 4 | 3 | 8 | 20 | |
| > 10 years | 1 | 6 | 10 | 9 | 26 | |
| Age of Patient (years) | ||||||
| 18 – 45 years | 8 | 1 | 8 | 5 | 23 | 0.974 |
| 46-60 years | 5 | 15 | 9 | 10 | 39 | |
| > 60 years | 10 | 6 | 10 | 8 | 34 | |
| Highest Education level | ||||||
| None | 3 | 0 | 1 | 4 | 8 | 0.778 |
| Primary | 10 | 15 | 15 | 9 | 49 | |
| Secondary | 8 | 6 | 4 | 7 | 25 | |
| Tertiary | 2 | 2 | 7 | 3 | 14 | |
| Last medication dose | ||||||
| Today | 16 | 10 | 13 | 10 | 49 | 0.857 |
| 1-2 days back | 4 | 5 | 12 | 9 | 30 | |
| 3-7 days back | 0 | 3 | 0 | 3 | 6 | |
| > 1 week back | 3 | 5 | 2 | 1 | 11 | |
| Fails to take medication | ||||||
| Yes | 2 | 5 | 3 | 4 | 14 | 0.655 |
| No | 21 | 18 | 24 | 19 | 82 | |
| Type of Medication | ||||||
| Oral hypoglycemic | 19 | 20 | 25 | 18 | 82 | 0.826 |
| Oral plus parenteral | 1 | 1 | 1 | 1 | 1 | |
| Parenteralonly | 3 | 2 | 1 | 1 | 4 | |
| Patient taking co-medication | ||||||
| Yes | 12 | 15 | 17 | 16 | 60 | 0.86 |
| No | 11 | 8 | 10 | 7 | 36 | |
| Has Medication Fatigue | ||||||
| Yes | 2 | 6 | 2 | 2 | 12 | 0.53 |
| No | 21 | 17 | 25 | 21 | 84 | |
| Experiencing Adverse effects | ||||||
| Yes | 4 | 5 | 7 | 7 | 23 | 0.277 |
| No | 19 | 18 | 20 | 16 | 73 | |
| Use of Local medicines | ||||||
| Yes | 5 | 5 | 5 | 6 | 21 | 0.812 |
| No | 18 | 18 | 22 | 17 | 75 | |
| Body Mass Index (BMI) | ||||||
| Underweight (< 18) | 2 | 0 | 0 | 0 | 2 | 0.451 |
| Normal (18-25) | 5 | 5 | 10 | 6 | 26 | |
| Overweight (35-30) | 9 | 6 | 3 | 7 | 25 | |
| Obese (>30) | 7 | 12 | 14 | 10 | 43 | |
Table 4: Factors associated with blood glucose levels among diabetic patients at Rubaga
Patients Medication Practices, Diabetes Care and Adherence to Diabetic Treatment (n =96)
(Table 5)
| Description | Number of Patients | Percentage of Patients |
| Day of last medication dose | ||
| Today | 49 | 51 |
| 1-2 days back | 30 | 31 |
| 3-7 days back | 6 | 6.3 |
| > 1 week back | 11 | 11.5 |
| Reason for not taking medication today | ||
| Adherent to dose | 66 | 68.8 |
| Medicine out of stock | 13 | 13.5 |
| Doctor’s Advise | 2 | 2.1 |
| Medication got finished | 1 | 1 |
| Forgot to take | 1 | 1 |
| Felt normal/healthy | 1 | 1 |
| Patient was fasting | 12 | 12.5 |
| Patient ever Failed to take medication | ||
| Yes | 14 | 14.6 |
| No | 82 | 85.4 |
| Reason for failing to take medication | ||
| Adherent | 83 | 86.5 |
| Medication got finished | 1 | 1 |
| On support medication | 1 | 1 |
| Medication fatigue | 4 | 4.2 |
| Not convenient | 1 | 1 |
| Use herbal remedies | 2 | 2.1 |
| Timing of treatment | 1 | 1 |
| Forgot | 1 | 1 |
| Stock out | 1 | 1 |
| Feltwell | 1 | 1 |
| Patients taking co-medications | ||
| Yes | 60 | 62.5 |
| No | 36 | 34.4 |
| Types of other medication used | ||
| None | 33 | 34.4 |
| Antihypertensive | 55 | 57.3 |
| Antibiotics (bone infection) | 1 | 1 |
| ART care | 2 | 2.1 |
| Headache medication | 2 | 2.1 |
| PUD treatment | 2 | 2.1 |
| TB medication | 1 | 1 |
| Patient ExperiencesMedication fatigue | ||
| Yes | 12 | 12.5 |
| No | 84 | 87.5 |
| Patient experiences adverse effects | ||
| Yes | 23 | 24 |
| No | 73 | 74 |
| Perceived cost of medication | ||
| Expensive | 67 | 69.8 |
| Affordable | 25 | 26 |
| Cheap | 4 | 4.2 |
| Perception of consultation time at hospital | ||
| Satisfactory | 90 | 93.8 |
| Fairly Satisfactory | 4 | 4.2 |
| Not satisfactory | 2 | 2.1 |
| Patient Know the name of medication | ||
| Yes | 24 | 25 |
| No | 72 | 75 |
| Patient believes in informal traditional treatments for diabetes | ||
| Yes | 25 | 26 |
| No | 71 | 74 |
| Patient uses local herbs or medicines alongside the medication given | ||
| Yes | 21 | 21.9 |
| No | 75 | 78.1 |
Table 5: Distribution of patients medication practices, diabetes care and adherence to diabetic treatment (n =96)
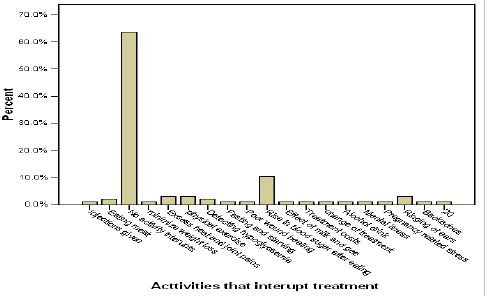
Factors that interfere with medication adherence (n =96)
(Figure 1)
Figure 1 : Activitiesthatinterrupttreatment
Health Practice by Diabetic Patients Attending Rubaga Hospital (n =96)
(Table 6)
| Foods patients avoid | ||
| Sweet foods | 62 | 64.6 |
| Starch foods | 10 | 10.4 |
| Sweet and starchy | 7 | 7.3 |
| No food should be avoided | 17 | 17.7 |
| Occasional eating habits | ||
| Yes | 73 | 76 |
| No | 23 | 24 |
| Last health education on diabetes | ||
| Never | 6 | 6.3 |
| Last visit | 62 | 64.6 |
| A number of visits a go | 22 | 22.9 |
| Today | 6 | 6.3 |
Table 6: Distribution on practices of diabetics patients
Discussion of Results
As a participant’s fasting blood glucose rose beyond the normal upper limits, so was their HbA1c value in excess of the study’s cut off of 6% thus revealing a strong association between the two (P=0.000). Our study findings revealed that there was poor glycaemic control in 58/96(60.4%) of the study participants which is a little higher than the 40% poorglycaemic control reported by Faiza, [16] but comparable with the findings of Sharon et al. [5].
No significant association was found between glycaemic control and gender (P value = 0.703) which agrees with the findings of Assiamira et al. [4], Sharon et al.[5] and Ana et al. [17] who also found no significant sex difference in the distribution of HbA1c levels for men and women. The findings are however contrary to those of Matthias et al. [18] who reported significantly poorer glycaemic control among male participants than their female counterparts.
A strong association was found between perceived high cost of treatment for diabetes mellitus and poor glycaemic control for the patient (P = 0.019). This made high cost of treatment a very strong predictor of poor glycaemic control of the patient, a comparable finding to those of Beran et al. [14].
Having another chronic disease requiring taking of medications alongside those of diabetes mellitus was significantly associated with poor glycaemic control (HbA1c levels above 6.0%) among this study’s participants (P = 0.045) and hence made it a predisposing factor for poor glycaemic control which is in agreement with the findings of Schectman et al. [10]. However, the general feeling of being tired of taking medicine was not significantly associated with high HbA1c levels above 6.0% (P = 0.877).
The duration one had spent with diabetes mellitus as per our study was not significantly associated with poor glycaemic control based on HBA1C levels of our study participants (P value = 0.81). This is contrary to the findings of Blaum et al. [19] and Stephen et al. [20] who reported that a long history of the disease was significantly associated with poor glycaemic control. However long duration of having diabetes mellitus was significantly associated with high fasting blood glucose concentrations (P = 0.003).
Age of our study participants was not related with glycaemic control in any way (P = 0.833). This is contrary to the findings of Nichols et al. [21] and Harris et al. [6] who reported that glycaemic control deteriorated with increasing age of the diabetic patient. It is also contrary in another way to the findings of Matthias et al. [18], who reported that glycaemic control improved with increase in the age of the diabetic patient.
No association was found between level of education of study participants and their HbA1c levels or glycaemic control (P = 0.426). This is contrary to the findings of Kalyango et al. [2], who noted in their study in part that patients with lower education levels and those with low socio-economic status had poor glycaemic control.
The treatment regimen the participant was on for their diabetes mellitus was not statistically related with their extent of glycaemic control (P value = 0.144). However, the fact that all of the study participants who were on both oral plus parenteral hypoglycaemics had high HbA1c levels relates with the findings of Sharon et al.,[5] who reported that taking of insulin alone or in combination with other drugs was significantly associated with poor glycaemic control among diabetic patients in their study.
Adverse effects of drugs for treatment of diabetes mellitus had no significant correlation with poor glycaemic control (P = 0.86) and is a contrary finding to that of Aburuz et al. [22], who reported poor drug compliance among diabetic patients attributed to its medication side effects.
No association was found between using informal herbal treatment and poor glycaemic control (P = 0.348). This is contrary to the findings of Pinkoane et al. [23] who reported that many a people with low socio-economic status in South Africa had poor glycaemic control because they preferred services of traditional and faith healers to the biomedical ones. Obesity reflected by a high BMI was not a predictor of poor glycaemic control in this study (P = 0.598). This is contrary to the findings of Nichols et al. [21] who reported that increase in body mass index (BMI) led to increased poor glycaemic control.
No association was found between time when the participant had had the last treatment for diabetes mellitus and their HBA1C levels (P = 0.325). Similarly, no association was found between occasional missing of DM treatment with HBA1C levels of the study
Conclusions
A high fasting blood glucose was predictive of a high HbA1c value and glycaemic control was poor but with no significant variation between the different gender.
Factors associated with poor glycaemic control in diabetic patients at Rubaga Hospital were high cost of treatment (P = 0.019), long duration of having diabetes mellitus (P = 0.003) and taking co-medication for another chronic illness alongside that of diabetes mellitus (P = 0.045).
In this study unlike in other studies, level of education of the study participants, type of treatment they were on whether oral or parenteral, adverse effects of drugs for their treatment, occasionally missing to take treatment, BMI and using of informal herbal treatment were not significantly associated with poor glycaemic control.
Recommendations
The government of the republic of Uganda through the ministry of health and other stake holders should make treatment of diabetes mellitus universally accessible and free even in private establishments like Rubaga Hospital in order to improve glycaemic control and minimise its deleterious effects.
Further research need to be done in health establishments in other parts of the country particularly in rural and semi-urban settings for a generalization to be made about the disease and its challenges.
References
- Lasky D, Becerra E, Boto W, Otim M, Ntambi J (2002) Obesity and gender differences in the risk of type 2 diabetes in Uganda. Nutrition 18: 417-421.
- Kalyango JN, Owino E, Nambuya AP (2008) Non-adherence to diabetes treatment at Mulago Hospital in Uganda: prevalence and associated factors. Afr Health Sci 8: 67-73.
- Ramnik S (2006) Text book of Medical Laboratory Technology-Diabetes mellitus laboratory diagnosis. New Delhi: Jaypee 1: 1291.
- Iribarren C, Karter AJ, Go AS, Ferrara A, Liu JY, et al. (2001) Glycaemic Control and Heart Failure Among Adult Patients With Diabetes. Circulation 103: 2668-2678.
- Saydah S, Cowie C, Eberhardt MS, De Rekeneire N, Narayan KM (2007) Race and ethnic differences in glycaemic control among adults with diagnosed diabetes mellitus in the United States. Ethn Dis 17: 529-535.
- Harris M, Eastman RC, Cowie CC, Flegal KM, Eberhardt MS (1999) Racial and ethnic differences in glycaemic control of adults with type 2 diabetes. Diabetes Care 22: 403-408.
- Melikian C, White TJ, Vanderplas A, Dezii CM, Chang E (2002) Adherence to oral diabetic therapy in a managed care organizations. J Clin Ther 24: 460-467.
- Shobhana R, Begum R, Snehalatha C, Vijay V, Ramachandran A (1999) Patients’ adherence to diabetes treatment. J Assoc Physicians India 47: 1173-1175.
- Whiting DR, Hayes L, Unwin NC (2003) Diabetes in Africa: Challenges to health care for diabetes in Africa. J Cardiovasc Risk 10: 103-110.
- Schectman JM, Nadkarni MM, Voss JD (2002) The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care 25: 1015-1021.
- Grant RW, Devita NG, Singer DE, Meigs JB (2003) Poly-pharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care 26:1408-1412.
- Raji A, Gomes H, Beard JO, MacDonald P, Conlin PR (2002) A randomized trial comparing intensive and passive education in patients with diabetes mellitus. Arch Intern Med 162: 1301-1304.
- Moreira ED Jr, Neves RC, Nunes ZO, de Almeida MC, Mendes AB, et al. (2010) Glycemic control and its correlates in patients with diabetes in Venezuela: results from a nationwide survey. Diabetes Res ClinPract 87: 407-414.
- Beran D, Yudkin JS, de Courten M (2005) Access to care for patients with insulin-requiring diabetes in developing countries: Case studies of Mozambique and Zambia. Diabetes Care 28: 2136-2140.
- Kish L (1965) Survey sampling. John Wiley & Sons, editor. New York: John Wiley & Sons.
- Faiza AQ (2005) Glycemic Control among Diabetics at a University and Erfan Private Hospital. Pakistan J Endocrinol Metab 2: 408-412.
- Mendes AB, Fittipaldi JA, Neves RC, Chacra AR, Moreira ED Jr (2010) Prevalence and correlates of inadequate glycaemic control: results from a nationwide survey in 6,671 adults with diabetes in Brazil. Acta Diabetol 47: 137-145.
- Matthias PHST, Christine XW, Helen SSL (2011) Association of Younger Age With Poor Glycaemic and Cholesterol Control in Asians With Type 2 Diabetes Mellitus in Singapore. J Endocrinol Metab 1: 27-37.
- Blaum CS, Velez L, Hiss RG, Halter JB (1997) Characteristics related to poor glycaemic control in NIDDM patients in community practice. Diabetes Care 20: 7-11.
- Benoit SR, Fleming R, Philis-Tsimikas A, Ji M (2005) Predictors of glycaemic control among patients with Type 2 diabetes: A longitudinal study. BMC Public Health 5: 36.
- Nichols GA, Hillier TA, Javor K, Brown JB (2000) Predictors of glycaemic control in insulin-using adults with type 2 diabetes. Diabetes Care 23: 273-277.
- Aburuz SM, McElnay JC, Millership JS, Smyth S (2002) Factors affecting self-care activities, postprandial plasma glucose and A1C in patients with type 2 diabetes. Int J Pharm Pr 10: 96.
- Pinkoane MG, Greeff M, Williams MJ (2005) The patient relationship and therapeutic techniques of the South Sotho traditional healer. Curationis 28: 20-30.