Case Report
Accidently Discovered Postpartum Pituitary Apoplexy after Epidural Anesthesia
Rafik Sedra
Anesthesia and Critical Care, Christie NHS Foundation Trust, United Kingdom
Corresponding author
Rafik Sedra, Department of Anesthesia and Critical Care, Christie NHS Foundation Trust, United Kingdom, E-mail: rookyloomy@gmail.com
Received Date: 15th September 2014
Accepted Date: 11th November 2014
Published Date: 13th November 2014
Citation
Sedra R (2014) Accidently Discovered Postpartum Pituitary Apoplexy after Epidural Anesthesia. Enliven: J Anesthesiol Crit Care Med 1(5): 014.
Copyright
@ 2014 Dr. Rafik Sedra. This is an Open Access article published and distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Anesthetic consideration of obstetric patients with pituitary disorders is an important topic to deal with. Few cases were reported with accidently discovered pituitary tumor complications especially in the postpartum period. A 26 years old primigravida lady with 39 weeks gestational period was reported to have severe headache and sudden loss of conscious after normal vaginal delivery with lumbar epidural anesthesia. Accidently discovered pituitary adenoma was proved after neurology, endocrine and ophthalmology consultations. Hence, undiagnosed pituitary adenomas should be taken in to consideration with unexplained postpartum generalized weakness and loss of conscious especially after exclusion of epidural anesthesia complications.
Keywords
Postpartum complications; Muscle weakness; Undiagnosed pituitary adenoma; Apoplexy
Abstract
Anesthetic consideration of obstetric patients with pituitary disorders is an important topic to deal with. Few cases were reported with accidently discovered pituitary tumor complications especially in the postpartum period. A 26 years old primigravida lady with 39 weeks gestational period was reported to have severe headache and sudden loss of conscious after normal vaginal delivery with lumbar epidural anesthesia. Accidently discovered pituitary adenoma was proved after neurology, endocrine and ophthalmology consultations. Hence, undiagnosed pituitary adenomas should be taken in to consideration with unexplained postpartum generalized weakness and loss of conscious especially after exclusion of epidural anesthesia complications.
Background
Many changes occur in pituitary gland during pregnancy; for instance, increase of volume, weight and height of pituitary gland throughout gestation [1]. The weight of the gland can increase up to (660-760 mg), also upward convexity increases homogenously. Volume of pituitary gland shows 30% increase in comparison to that measured in pregestational period [1,2].
Pituitary volumes and infundibulum increases enormously in the first three days after delivery. The height of the pituitary gland can increase up to 12 mm during the postpartum period, whilst normal physiological dimensions will be restored within six months after delivery [3]. Physiological changes occurring during pregnancy affect the pituitary gland to a great extent. These changes are mainly due to pituitary and placental hormones. There is an increase in lactotroph cells which is mainly due to estrogen besides elevation of prolactin near the end of pregnancy. On the other hand, gonadotropin levels decrease throughout pregnancy, level decline starts from 6 weeks of gestation. Furthermore, gonadotroph releasing hormone is not affected by gonadotropins, but it is mainly influenced by estrogen, progesterone and prolactin feedback mechanism. Somatotroph cells also decrease throughout pregnancy which leads to decreased growth hormones levels and increased insulin growth factor-1, all these changes happen due to release of placental growth hormone [1,4].
Case Report
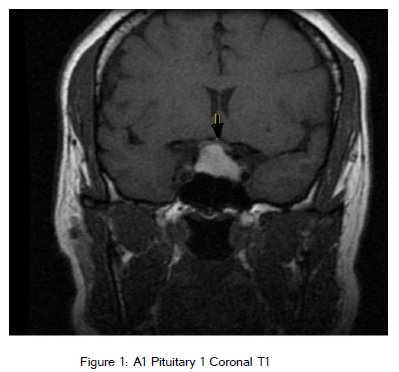
A 26 year old primigravida lady, 39 weeks gestational period was admitted in emergency department at St.Peter specialised hospital in Cairo, Egypt with labour pains. The Obstetrician confirmed that the patient is in labour and vaginal examination was done which showed cervical dilatation of 4 cm, and living fetus was confirmed with ultrasound examination. The lady had regular antenatal care and nothing was relevant in her past medical, drug and surgical history. Obstetrician notified the anaesthetist for epidural anaesthesia for normal vaginal delivery as the patient is in active labour. Patient’s Blood pressure was 130/75 mmHg and pulse was 110 beats/min of sinus rhythm. One liter of hartmann solution was infused before epidural insertion and Epidural procedure, benefits and complications were explained to the patient. Patient's back was sterilized. Local anesthesia skin infiltration with 1% lidocaine at level of L2-L3 was done. Dural puncture was made with epidural tuohy needle. After local anesthesia infiltration, epidural needle was removed and inserted again at high level (L1-L2) after local anesthesia infiltration. As a second attempt, Epidural space was reached at 4cm, catheter to skin distance was 10 cm, epidural space was reached. Neither cerebrospinal fluid nor blood was out after aspiration. Test dose of 3 cm and 1% lidocaine was given without any heaviness in lower limbs or changes in blood pressure. Then loading dose was given with bupivacaine 0.125% (10ml) and 50 ug fentanyl. Patient position was semi-setting. Patient started feeling heaviness in her lower abdomen, buttocks and lower limbs after 10 mins. There was a fall in blood pressure to 100/50 mmhg, with pulse of 100 beats/min. Sensory level test was done and found to be at T8, with slightly motor affection at both lower limbs. Patient was informed about the dural puncture and possibility of high headache. Urinary catheter was inserted and pain was controlled by epidural syringe pump with bupivacaine 0.125% at rate of 6ml/hr. Blood pressure was measured for every 5 minutes with crystalloid fluids infuse and continuous fetal monitoring. Blood pressure was maintained with fluids without need of vasopressors. Six hours later, patient cervical dilatation reached 9 cm, and patient was moved to operating theater. 8 ml of 0.125% bupivacaine was given in epidural catheter by anesthetist and the patient was free from pain with slight motor affection at lower limbs where she delivered a baby normally after 15 minutes and baby was examined by the neonatologist. Then 3 mg of midazolam was given to patient with slow infusing 30 IU of oxytocin. The Patient was vitally stable with blood pressure (110/60 mmHg), pulse of 90 beats/min, and with normal sinus ECG. Then the patient was a bit drowsy but was in good condition and was moved to ward. By injecting 2 mg morphine in epidural catheter, on the same night epidural catheter was removed (Figure 1).
Next day afternoon, the patient complained with severe headache, general weakness and episode of loss of conscious for few seconds. The Anesthetist was called to review the patient. NSAID and paracetamol were given with encouragement of oral fluids for severe headache. On first postoperative day, Neurological consultation, sensory and motor examination was done to know level of epidural block, but the patient was found to have intact sensory and motor sensation. Patient had no history of any muscle or neurological disease. On third postoperative day, patient still complained restricted peripheral vision with an episode of conscious loss for few seconds, but the headache was not severe as the first postoperative day. Ophthalmology consultation was done showing bitemporal hemianopia with macular sparing. Pituitary macroadenoma with hemorrhagic pituitary apoplexy was found on Magnetic Resonance Imaging (MRI). Endocrine investigations showed normal Prolactin level (190 ng/ml), dexamethazone suppression test showed normal cortisol level (137 nmol/l), Insulin growth factor-1 was normal as well (15 nmol/l, normal reference 13-37 nmol/l), Symptoms got resolved spontaneously after two weeks; repeated MRI scan showed decrease in pituitary adenoma . Visual field tests were repeated regularly showing great improvement, patient restored her normal visual field after 2 weeks. Prolactin level test was repeated again after one week where the result was normal (120 ng/ml). Six months later, Patient stopped breastfeeding and regained regular menstrual cycles. Endocrinologist recommended MRI brain follow up yearly and conservative treatment.
Discussion
Accidental Dural puncture after epidural anesthesia is a serious complication with patient having high intracranial pressure. After the patient developed episodes of loss of conscious with severe headache the day after normal delivery, the main concern was, is it related to lumbar epidural dural puncture or not? Dural puncture with high intracranial pressure can cause brain stem herniation due to CSF leakage and sudden decrease of intracranial pressure [7]. The anesthetist gave strong pain killers to the patient and more fluids to relief the headache. Eventually, Headache got improved a little bit but patient still suffered from bitemporal hemianopia and episodes of loss of conscious. On the other hand, there was no history of infertility, dysmenorrhea, and osteoporosis so prolactinomas were excluded. Also, no history of soft tissue enlargement, increased sweating, coarse features, and growth hormone secreting adenomas got excluded. No hypertension, diabetes mellitus, moon face & the only signs we got are episodes of loss of conscious and even restricted visual field was not that severe [5]. When neurological consultation was done, the neurologist decided to go for MRI brain. Scan was done showing a mass in sella turcica which was confirmed by radiologist to be a pituitary macroadenoma with hemorrhagic apoplexy, exclusion of brain herniation done as well. Endocrinologist consultation was done who diagnosed this lady with pituitary non secretory apoplexy, laboratory results showed normal levels of free T3, blood glucose and cortisol. The diagnosis was reached after reviewing patient's history, clinical presentation, MRI brain and laboratory results. Pituitary apoplexy incidence is about 10% of pituitary adenomas, has 2 types haemorrhagic or ischemic due to infarction [6]. Symptoms got improved spontaneously after two weeks without any medical or surgical interference.
Conclusion
Pituitary adenomas should be taken in consideration especially with postpartum bitemporal hemianopia and disturbed conscious level. Exclusion of other differentials should be done first especially epidural complications. Neurology and endocrinology consultations needed to be done as soon as possible.
References
2) Molitch ME (2003) Pituitary tumors and pregnancy. Growth Horm IGF Res Suppl A: s38-s44.
5) Tatter SB (2007) Pituitary tumour symptoms.